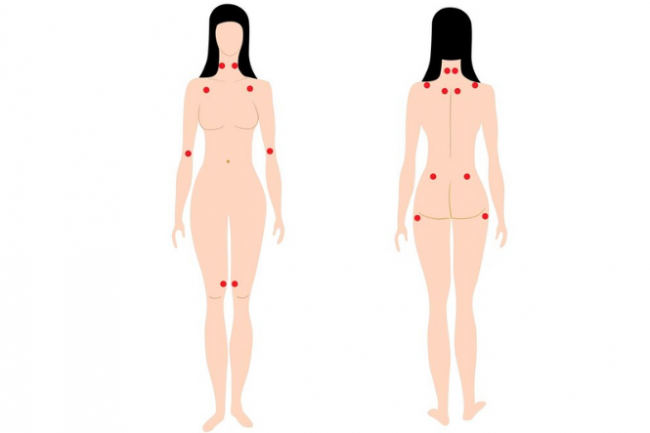
- Fibromyalgia is a term used to describe widespread pain and tenderness in different areas of your body.
- It is thought to be a disorder of the way your brain and nervous system receive and interpret signals for your body, resulting in pain.
- Fibromyalgia is very common, with a prevalence of about 2%. Women are 7 times more likely than men to be affected.
- Fibromyalgia is a long-term (chronic) condition – pain and discomfort often extends beyond 3 months. There may be periods when symptoms flare up or times when they become more manageable.
- People with fibromyalgia often experience other symptoms, eg, fatigue, poor sleep, difficulty concentrating and sensitivity of their bladder and bowels.
- Fibromyalgia can be hard to understand and difficult to explain to those close to you. Some people might find the diagnosis difficult to accept. Most people find ways to feel well and take note of what exacerbates their symptoms, so they can continue to do what they love while living with fibromyalgia.
- The goals of treatment are to avoid triggers that flare up bouts of pain and to feel supported in activities that improve your sleep and increase your ability to do the things you want to do, while also reducing your pain and other symptoms.
- Medicines are not effective in treating fibromyalgia but may play a role in reducing the associated symptoms. With the right combination of therapies and lifestyle changes, it's possible to live well and manage the symptoms of fibromyalgia.
Fibromyalgia is not your fault
You haven't caused this condition yourself, nor is it 'caused' by anxiety or depression. Instead, recurring pain is a neurophysiological problem of the nervous system or pain system that can be identified and treated.
- Your pain and/or symptoms are totally real – they're not made up or in your head.
- It's not your fault that you have fibromyalgia.
- You're not psychologically unwell.

Image credit: Canva