There are many ways to treat nerve pain. The first step is to see your doctor and treat the underlying cause (if there is one). For example, better control of diabetes can also help to improve pain from diabetic neuropathy.
The main aim of treatment is to keep you active and engaged in your daily activities. Treatment may include a combination of medication and non-medication options.
Non-medication approaches
- Acupuncture or transcutaneous electrical nerve stimulation (TENS) may be useful some people.
- Psychological approaches, such as cognitive-behavioural therapy (CBT), may help some people to adapt to living with pain. However, there is little evidence to suggest it reduces neuropathic pain.
- Have a plan for how to manage your daily activities. People with long-term pain often tire quickly and planning your activities can enable you to have a greater sense of control over your condition. You may want to devote time to important tasks early in the day or when you have the most energy.
- Try to get enough sleep. Poor sleep can make pain worse, but pain can disrupt your sleep. Talk to your doctor if you are having problems sleeping.
- Keep active. Keeping active is very important – simply being inactive can cause pain. A physiotherapist may be able to assist you with suitable exercises and advise you on how to become more active without aggravating your pain.
- Learn about mindfulness. Mindfulness reduces stress, tension and anxiety. It can help you to avoid focusing too much on your pain as well as directing your thoughts in a way that is helpful to manage your pain.
Read more about non-medication treatments for pain.
Medications
Regular painkillers do not usually work for nerve pain. These include paracetamol, NSAIDs such as ibuprofen and diclofenac and opioids such as codeine.
Other medicines that have been found to be more effective in relieving nerve pain, include:
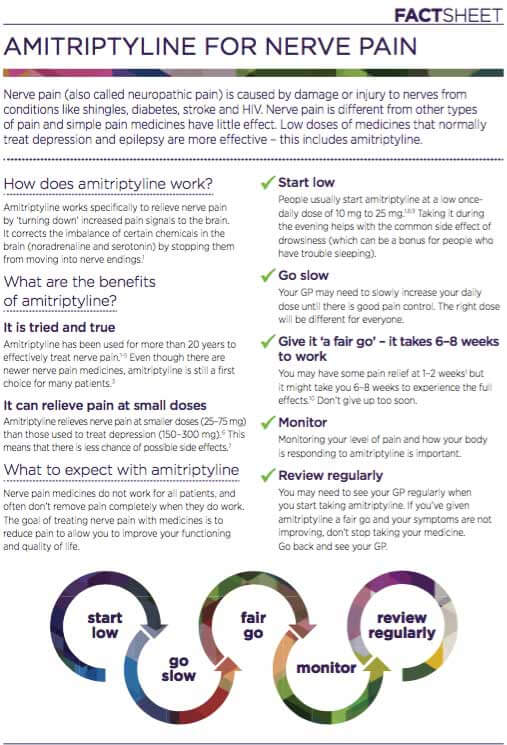
These medications often need to be taken for a few weeks before you experience optimal pain control. If your pain does not respond to one option, your doctor may suggest changing to another or combining more than one medication. Your doctor will start you on a low dose and gradually increase the dose until you notice an effect. Higher doses may be more effective, but are also more likely to cause side effects. The most common side effects are tiredness, dizziness, feeling drowsy and lack of concentration. If you get these, it may be necessary to reduce your dose. Don't drive or operate machinery if you experience drowsiness or blurred vision. You also may become more sensitive to the effects of alcohol.
Another treatment option is the use of capsaicin cream, where a small amount of cream is rubbed on the painful area of skin three or four times a day. This is useful if your pain is confined to a particular area of your body, or if you cannot take the medicines above. Capsaicin is the substance that makes chilli peppers hot and is thought to work in neuropathic pain by stopping the nerves sending pain messages to the brain. Read more about capsaicin cream.