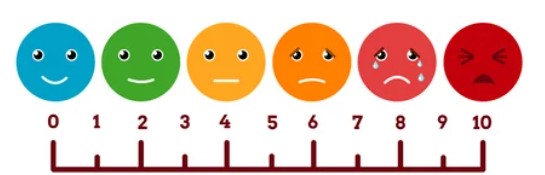
Your health professional might ask you to rate the intensity of your pain (how bad it is) by choosing a number on a scale from 0–10. On this scale 0 out of 10 indicates that you have no pain at all, and 10 out of 10 means the worst possible pain. The middle (around 5) is moderate pain.
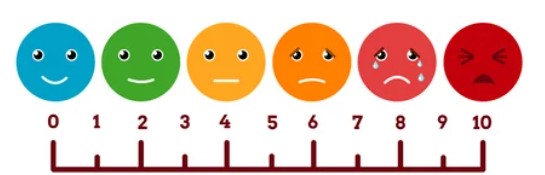
Image credit: 123rf
You may be asked to rate your pain using the pain scale for your “best” day, “worst” day, and on an “average” day. This helps your health professional get a clear picture of how your pain level changes each day.
Sometimes people have trouble describing their pain, this may apply to young children, people with intellectual difficulties, or where there are language barriers or communication difficulties. In these cases, your healthcare provider may use other signs to gauge pain. These include:
- crying
- facial changes (eg, grimacing or frowning)
- changes in sleeping or eating patterns
- becoming quiet and/or withdrawn
- screaming or refusing to move.
The faces pain scale, as pictured above, can also be used. The person in pain can point to the facial expression that represents how their pain makes them feel.