This page focuses on asthma in adults. For information about children with asthma, see asthma in children.
Low or no data? Visit zero.govt.nz, scroll down the page then click on our logo to return to our site and browse for free.
Asthma in adults
Key points about asthma in adults
- Asthma (mate huango) is a common lung condition that affects the breathing tubes (airways) that carry air in and out of your lungs.
- Asthma causes wheeze and cough, and can make it difficult to breathe.
-

Video: What is asthma?
This video is about your lungs and how asthma affects them. It may take a few moments to load.
- New Zealand has one of the highest rates of asthma in the world, affecting up to 1 in 7 children and 1 in 8 adults.
- If you have asthma, your airways are sensitive and react to certain triggers such as allergens (substances that cause an allergic reaction), viruses, cold or humid weather, exercise and air pollutants such as cigarette smoke.
- These triggers cause your air passages to tighten up, swell on the inside (become inflamed) and produce more mucus.
- As a result, the airways become narrower, making it difficult for air to move into your lungs, and even more difficult for air to move out.
- Learning about asthma, what causes it and how it is treated can help you avoid triggers and keep your symptoms under control.
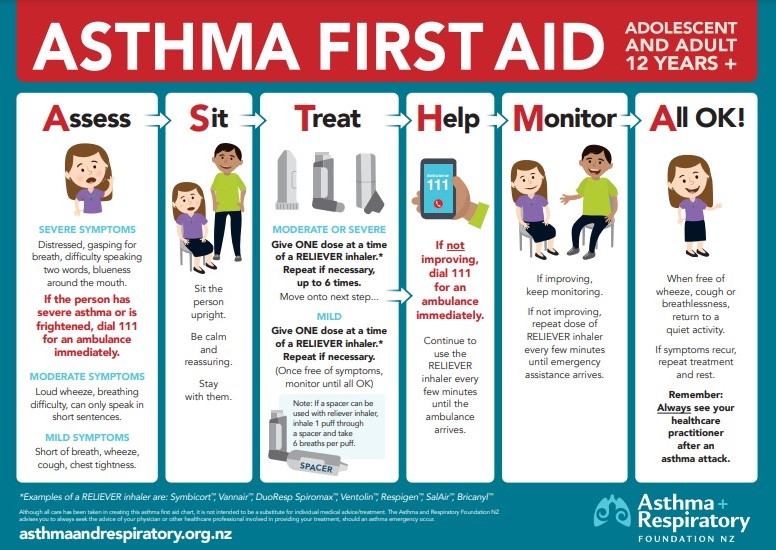
- Seek urgent medical help if you have severe asthma symptoms.
Asthma is thought to be caused by a combination of genetic and environmental factors.
Genetic factors
Asthma and allergies are closely linked. About 70 to 80% of asthma in New Zealand is associated with allergies. Often people with asthma also have eczema (allergic skin rash) or hay fever, or have close family members who have asthma, eczema or hay fever. The tendency for these 3 conditions to occur together is known as atopy. If you are atopic, allergies can be a trigger for your asthma.
Environmental factors
Certain things in our environment thought to have a role in causing asthma include:
- allergens
- air pollution (such as tobacco smoke or petrol fumes)
- workplace chemicals.
(Asthma NZ, UK, 2021)
Asthma is ongoing and your symptoms may come and go.
Common symptoms of asthma include:
- difficulty breathing, feeling out of breath or as though you can't get enough air out of your lungs
- a tight feeling in your chest like something is squeezing or sitting on your chest
- wheezing (a whistling, musical or squeaky noise in your chest)
- a cough, which can be worse at night or in the morning.
If you have any of these symptoms, see your doctor so they can assess if this is due to asthma or something else.
|
Severe asthma symptoms |
|---|
|
From time to time, your symptoms may get gradually or suddenly worse. Seek urgent medical help if you have any of these severe symptoms:
|
Learning what triggers your asthma and finding ways to avoid or reduce the effects is an important part of managing your asthma.
Common asthma triggers include:
- house dust mite
- infections of the airways, such as colds and flu
- pollen or mould
- pets
- cigarette smoke
- weather, such as change in temperature, cold weather or humid weather
- exercise
- stress and high emotion
- chemicals that irritate the airways, such as sprays, perfumes, cleaning fluids
- some medications (read more about medications that may trigger asthma).
In most cases, asthma can be diagnosed from:
- a description of your asthma symptoms now and in the past
- listening to your breathing with a stethoscope
- checking how your lungs are working with breathing tests, such as a peak flow meter (a device that measures changes in your breathing over the day) and spirometry (a machine that measures lung function).
In some cases, more detailed testing may be required, such as a skin-prick test to test for allergens or, rarely, a chest x-ray to rule out other conditions.
Once a diagnosis is made, your doctor will prescribe the type of medicines you need to take and will set up an asthma action plan(external link). This plan reminds you how to manage your asthma every day and how to recognise and manage your asthma when your symptoms get worse.
While asthma cannot be cured, the correct use of medicine combined with other self-care measures means that symptoms can be well controlled in most people.
Asthma treatment aims to keep your symptoms under control and prevent asthma attacks or sudden worsening of symptoms, so that your asthma does not interfere with your daily activities and you can enjoy a full and active life.
Generally there are 2 main approaches to the treatment of asthma, depending on whether you are using a budesonide/formoterol inhaler or a steroid inhaler with/without long-acting bronchodilator.
Budesonide/formoterol
|
Budesonide/formoterol |
|
Mild symptoms
|
|
Moderate to severe symptoms
|
Steroid inhaler with/without long-acting bronchodilator
| Steroid inhaler with/without long-acting bronchodilator | |
Mild symptoms
|
|
Moderate to severe symptoms
|
In severe exacerbations of asthma, a doctor may prescribe prednisone for a short period which is a tablet to help reduce inflammation. There are other less commonly used medications for asthma prevention such as montelukast tablets.
Flu vaccine
People with asthma are at increased risk of complications from the flu, even if their symptoms are mild or well-controlled by medicine. Complications include pneumonia (lung infection), heart failure and worsening asthma symptoms. The flu is also associated with increased risk of hospitalisation for people with asthma.
- Ask your doctor about getting the flu vaccination to reduce your risk of flu.
- The flu vaccine is usually free for people with asthma, if you are on regular preventative therapy.
- It is best to get vaccinated before the start of the winter season, before the flu enters the community.
- It’s important to get the flu jab every year because each year the flu vaccine is developed to match the different strains of flu virus you are likely to come across.
- Read more about influenza and the flu vaccine.
- Keep an eye on your symptoms. If you are getting wheezy more than 2 times a week, it may mean your asthma is not well controlled. See your doctor for a check-up.
- If you have symptoms of hay fever (allergic rhinitis), such as nasal congestion, runny nose, sneezing and itchy eyes, talk to your doctor about medicine to treat these symptoms, such as antihistamines or nasal steroid sprays. Treating hay fever can improve your asthma symptoms.
There are many things you can do to improve how well your asthma is controlled. By working with your doctor or nurse to create an asthma action plan(external link), you can reduce how bad your asthma symptoms are and how often you have them.
- Understand your asthma and learn to recognise your symptoms and your triggers.
- Take your prescribed medicine, especially your preventer, every day, regardless of whether you have asthma symptoms or not.
- If you smoke, try to quit. Try to keep clear of anyone else who smokes and of any other fumes.
- Ask your doctor about managing allergies if these are a known trigger for you.
- Use the asthma under control test(external link)(external link) to check if your asthma is well controlled or not.
- Use a peak flow meter to take and record regular readings to check that your asthma is under control.
- Keep active – physical activity improves how well your lungs work, and people who are fit usually find they have less asthma and cope better when they do have it.
- Visit your asthma team (your GP, your practice nurse and your pharmacist) regularly. They will review the medicines you are taking and can teach you how to use your inhaler properly so you get the most benefit.
- Keep your dust-mite allergy under control.
Read more about an asthma action plan.(external link)
Support
Asthma New Zealand provides education, training and support to individuals with asthma/COPD and their families. Read more(external link)(external link).
Cheyanne’s story – mum’s first time experience with life-threatening asthma
Cheyanne tells her story of the near-death experience by asthma of her daughter Ngamihi.
Cheyanne McConnell from Hamilton has two beautiful daughters. Her oldest is Ngamihi Lyndon, who has asthma, and Anahera Lyndon is the younger of the two. Cheyanne is deaf, therefore uses sign language, and Ngamihi helps her as a sign language interpreter. Cheyanne describes Ngamihi as really lovely and very amazing for doing this. She says both her daughters are really sweet girls.
Unfortunately, in early 2015, Cheyanne and her family had a frightening experience with asthma. Ngamihi was in a serious condition and needed to be taken to the hospital. Cheyanne explains, “It was very hard for my daughter Ngamihi, she nearly died. I took her straight to the hospital. I’m very lucky. I feel shocked that Ngamihi had asthma.”
The whole experience was incredibly emotional and traumatising. “Ngamihi in hospital made us all cry, she nearly died. She had fallen down, she was wheezing and upset crying. She had a hard cough and dry throat," says Cheyanne. This was Cheyanne’s first time in dealing with asthma, as she had never experienced it before and didn’t know anything about the condition.
To learn more about asthma, Cheyanne got in contact with Asthma Waikato to book an appointment for one-on-one asthma education. Cheyanne says, "I need to learn more about asthma for my daughter Ngamihi. It's very important".
Cheyanne recently completed her training with a very positive experience. She says about her asthma educator, Victoria Johnstone, "She's very great. I like to learn about asthma, it helps me understand. The training worked out all good." This education will help her look after and manage Ngamihi’s asthma.
Asthma societies such as Asthma Waikato offer friendly, specialised support, information and resources to assist people manage their respiratory condition. If you'd like to get in touch with an asthma society in your region, view the list of asthma societies in Aotearoa New Zealand.(external link)
Alistair's story – ironman and asthmatic
Alistair is a chronic asthmatic, but he’s also an Ironman. He’s had a few health challenges but he’s learned ways to manage his condition so he can compete at a high level in a triathlons.

"My childhood was punctuated with time in and out of hospital, although my parents were proactive in sourcing the best treatments available, including my very own nebuliser," he says.
"My asthma is at the worst end of the scale: it’s severe, especially if I don’t do my best to control it. Many things cause my asthma and even when it’s managed well, there are certain triggers that all the control in the world won’t stop an attack from coming on.
In late 1999 I was introduced to triathlons. It was not long before I was hooked and in 2005 I made the NZ Age Group Team for the Triathlon. In 2006 I took time out from sport. By 2009 I was struggling to do anything in the way of activity that lasted longer than 20 to 30 minutes, without the need for my reliever inhaler.
After having a lot of time off (three to four years) I was 25 kg heavier and much older. I realised then my triathlon training had helped me take control of my asthma in a way no other sport had ever done. I knew I had to get back into it, which meant I had to build up my training slowly and steadily.
Given how severe my asthma is, it’s crucial I manage myself well. Additionally, the sport I do has me actively engaging with asthma triggers on a daily basis. The key stages to my successful management have been:
- Regular visits to my health practitioner (I used to go every six months but now I am down to yearly, which is an excellent sign that I am more in control of my asthma).
- Undertaking tests to confirm what triggers my asthma. Some I class as core triggers (they trigger me no matter what), and the rest I class as secondary triggers (these can be managed by lifestyle and adaption).
- Getting onto the right medication for my asthma.
- Ensuring I am taking my preventative as prescribed.
- Constantly monitoring to understand what I feel like when I require my blue inhaler, and observing what is going on with me and the environment when this occurs.
Successful management of asthma has been a lifestyle choice. I know it works, because when I choose to alter my lifestyle I see and feel the difference in my asthma. I am proof that no matter how severe your asthma condition is, there is a way to take back control of your asthma and your life."
Alistair 'Ironman for Asthma' generously fundraises for The Asthma & Respiratory Foundation NZ, as well as raising awareness of asthma in the community. For more information on Alistair and how to support him, visit his Ironman for Asthma Facebook page/.(external link)
To help manage your or a family member's asthma, it's important to have an asthma plan(external link) in place. See your doctor and ask for an asthma plan.
Information sourced from Asthma & Respiratory Foundation NZ(external link)
It can be hard to remember directions or instructions from your healthcare provider. That's why you also need an asthma action plan. This is a written document to help you remember what you need to do to manage your asthma well.
It includes information on how to:
- manage your asthma daily, including taking medications correctly
- identify and avoid exposure to allergens and irritants that can bring about asthma symptoms
- recognise and handle worsening asthma symptoms, and when, how, and who to contact in an emergency.
You can develop your asthma management plan with your healthcare provider. It will be based on how severe your asthma is and your preferences. At each visit with your healthcare provider, you can review your plan and make changes as needed.
What are the benefits of an asthma action plan?
Using an asthma action plan that meets your individual needs has been found to:
- reduce absences from work or school
- reduce hospital admissions
- reduce emergency visits to general practice
- reduce reliever medication use
- improve lung function.
Sample asthma action plans
Note: Some of these resources are from other countries so make sure you know the emergency numbers for New Zealand. Ring 111 for emergencies or Healthline 0800 611 116.
Find Asthma Management plans for adults and children on this page.(external link)
New Zealand Sign Language videos about chest pain, produced by Platform Trust, in partnership with Deafradio and Healthify He Puna Waiora, NZ.
These videos are NZSL translations of Healthify pages on asthma. They may take a few moments to load.
Video: Asthma – an overview
(Platform Trust, in partnership with Deafradio and Healthify He Puna Waiora, NZ, 2022)
Video: What causes asthma?
(Platform Trust, in partnership with Deafradio and Healthify He Puna Waiora, NZ, 2022)
Video: What are symptoms of asthma?
(Platform Trust, in partnership with Deafradio and Healthify He Puna Waiora, NZ, 2022)
Video: What triggers asthma symptoms?
(Platform Trust, in partnership with Deafradio and Healthify He Puna Waiora, NZ, 2022)
Video: How is asthma diagnosed?
(Platform Trust, in partnership with Deafradio and Healthify He Puna Waiora, NZ, 2022
Video: How is asthma treated?
(Platform Trust, in partnership with Deafradio and Healthify He Puna Waiora, NZ, 2022)
Living with asthma(external link)(external link) Asthma & Respiratory Foundation NZ
Breathe better september(external link)(external link) Asthma & Respiratory Foundation NZ
Family health history(external link)(external link) Genetic Science Learning Centre, University of Utah, US, 2015
Rhinitis and asthma – combined allergic rhinitis and asthma syndrome(external link)(external link) World Allergy Organization
Tools and resources(external link)(external link) Centre of Excellence in Severe Asthma, Australia, 2018
Resources
Note: Some resources below are from overseas so some details may be different in New Zealand, eg, phone 111 for emergencies or, if it’s not an emergency, freephone Healthline 0800 611 116.
Brochures
- Asthma - what is it?(external link)(external link), Asthma and Respiratory Foundation NZ, 2013
- Inhaler chart(external link)(external link), Counties Manukau Health, NZ, 2021 [PDF, 655 KB]
- Erin & Isaac's healthy lung tips(external link) Asthma and Respiratory Foundation of NZ
- Asthma – First aid poster(external link)(external link), Asthma and Respiratory Foundation NZ, 2021English(external link), Māori(external link)
- GINA patient guide for asthma – you can control your asthma(external link), Asthma Respiratory Foundation NZ, 2020
- NZ adolescent and adult asthma guidelines(external link)(external link), Asthma Respiratory Foundation NZ, 2020
- Asthma checklist(external link), Asthma Respiratory Foundation NZ
- Breathing and asthma(external link)(external link), Asthma Respiratory Foundation NZ, 2010
- House dust mites(external link), Asthma Respiratory Foundation NZ, 2010(external link)
- Asthma – help yourself and stay well Asthma & Respiratory Foundation NZ English, (external link)te reo Māori(external link)
- Triggers in asthma Asthma & Respiratory Foundation NZ Webpage and booklet(external link)
- Better breathing – healthy lung checklist Asthma & Respiratory Foundation NZ Better breathing brochure(external link)
- Home sweet healthy home Asthma & Respiratory Foundation NZ Home sweet healthy home brochure(external link)
- Impact of respiratory disease in NZAsthma & Respiratory Foundation NZ Impact of respiratory disease in NZ brochure [PDF, 295 KB]
Apps/tools
There are variety of mobile apps available for people with asthma. These can be a useful way to learn about and take control of your asthma, eg, they can help you keep track of your symptoms, triggers, peak flow readings and medication. You can also create an asthma action plan together with your doctor or nurse. The Healthify app library team has reviewed some asthma apps that you may like to consider. Read more about asthma apps(external link).
References
- Barnard LT, Zhang J. The impact of respiratory disease in NZ – 2018 update(external link)(external link) Asthma and Respiratory Foundation NZ, 2018
- NZ adolescent and adult asthma guidelines 2020(external link)(external link) Asthma + Respiratory Foundation, NZ
Brochures
Asthma and Respiratory Foundation NZ, 2013
Asthma & Respiratory Foundation, NZ
Māori(external link), Samoan(external link)
Asthma and Respiratory Foundation NZ, 2021
English(external link), Māori(external link)
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Donny Wong, Respiratory Physician, Auckland
Last reviewed:
Page last updated:





