Eczema is associated with having an impaired skin barrier (‘sensitive skin’). With the most common form of eczema, called atopic dermatitis, there is often a family history of eczema, hay fever and/or asthma.
Low or no data? Visit zero.govt.nz, scroll down the page then click on our logo to return to our site and browse for free.
Eczema | Mate harehare
Also known as atopic dermatitis
Key points about eczema
- Eczema (mate harehare) is a common skin condition that causes redness, inflammation, dryness and itching of your skin.
- Eczema is commonly found behind your knees and on your arms, hands, neck and face.
- Eczema is not contagious.
- Eczema can be mild, moderate or severe and can go through phases.
- Management of eczema involves avoiding things that make it worse, using moisturisers and correct use of corticosteroid creams.
- Antibiotics may be needed if your skin becomes infected.

Eczema is more common in babies and children than adults, as many people find eczema improves as they get older.
Eczema in babies
- Eczema in babies (known as infantile eczema) usually starts between 4 and 6 months of age when the baby develops a red itchy rash, which may weep.
- The rash appears on the cheeks and may spread to the forehead and the backs of arms and legs.
- In severe cases, it may involve the whole body. Heavy scaling similar to cradle cap may occur.
- In some cases eczema improves after the age of 1 year. However it has the potential to persist or recur in later life.
Eczema in children
- Childhood eczema may follow the baby phase almost immediately, or it may start for the first time between the ages of 2 and 4 years.
- In childhood eczema, the rash is found in the creases of the elbows, behind the knees, across the ankles and wrists, and may involve the face, ears and neck as well.
Read more about eczema in babies and children.
Eczema in adults
- Adult eczema usually has large areas of very itchy, reddened, weeping skin with your elbow creases, wrists, neck, ankles and behind your knees being especially affected.
- It may be provoked by sunlight or exposure to environmental allergens.
- Adults who have had childhood eczema are more likely to suffer from hand dermatitis (due to contact with irritants and allergens).
- Eczema tends to improve in middle life and is unusual in elderly people.
The following factors can all make eczema worse:
- dry skin
- hot weather, high humidity and perspiration from exercise
- being unwell eg, having a common cold or stress
- skin infections caused by bacteria or viruses
- contact with things in the environment that cause an allergy (called allergens) such as dust, grass, wool or pet fur
- chemicals that irritate skin, such as those found in detergents and other cleaning products
- teething in babies
- children with eczema are at increased risk of developing food allergy, but the food doesn’t cause the eczema. Instead, some foods can cause irritation or a delayed eczema flare, eg citrus or tomatoes.
There is currently no cure for eczema, but there are many ways of controlling the symptoms. If you manage your eczema well with the appropriate treatment and self-care, it should improve over time. Do the following to help keep eczema under control.
Avoid irritants and triggers
Avoid things that make your eczema worse (flare up). Common irritants (known as triggers) include soap, detergent, wool and heat. Once you know your triggers you can try to avoid them. For example, wear soft cotton and keep room temperatures cool.
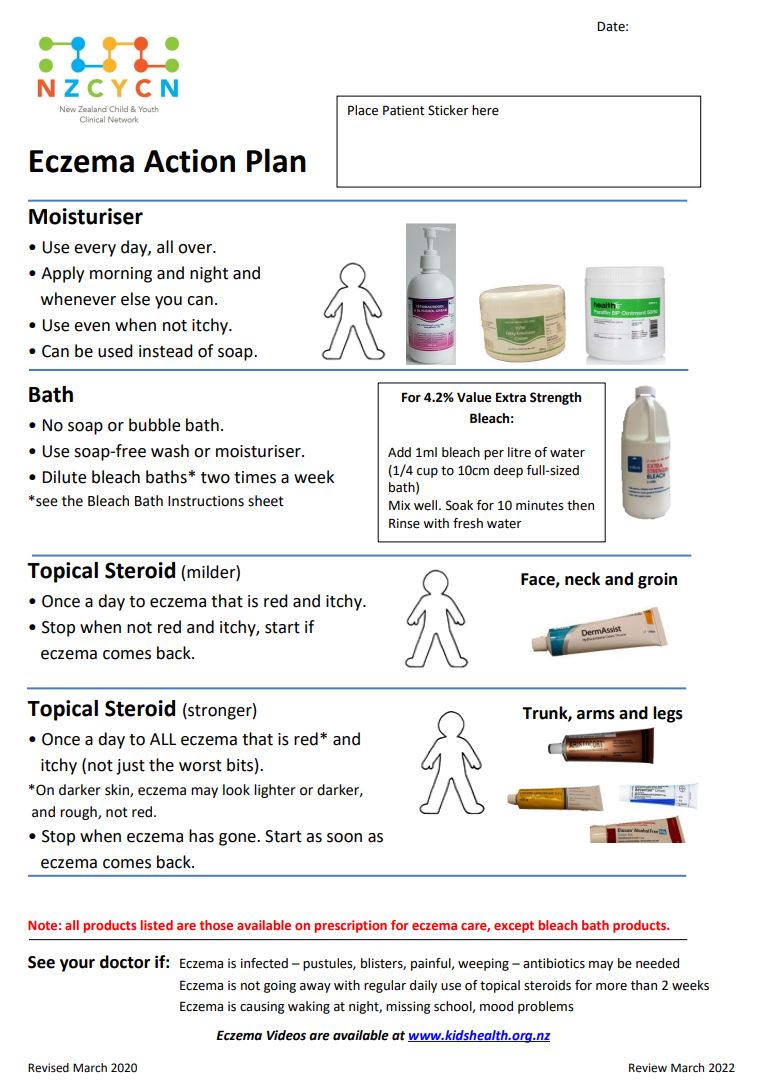
Bath or shower every day to help keep your skin moist and clean
Have a bath or shower every day to help moisturise your skin. Limit bathing time to 10 to 15 minutes and try not to have the water too hot as it can dry out and irritate your skin.
- Use soap substitutes such as sorbolene. You can apply this to your skin before bathing then wash it off. You can buy these without a prescription.
- Avoid soap (including liquid soap) as it can dry out your skin.
- Avoid using bubble baths, which can be extremely drying and irritating. Instead try bath oils which can hydrate your skin, coating it with a film of oil to trap water in the skin. You can buy bath oils or dissolve a teaspoon of emulsifying ointment under the hot tap.
- If your scalp is affected use a less irritant shampoo such as E45 Dry Scalp Shampoo. T-Gel is a gentle tar shampoo that may help treat dry scalps.
- Avoid hair conditioner as it can cause irritation.
- If you get infected eczema often, it may help to add an antiseptic to the bath such as Oilatum Plus or QV flare up. Don’t use though more than once a week. These products can be quite expensive. An inexpensive option is a bleach bath. Bleach comes in different strengths. This factsheet(external link) tells you how much to use. Don't have a bleach bath more than twice a week.
Use moisturisers (emollients) regularly
Keep your skin moist by using moisturiser regularly two to three times a day or as frequently as needed to keep your skin moist. It's important to use moisturisers all the time, not just when you have symptoms.
- When you apply moisturiser, smooth it onto the skin in the direction that your hair grows.
- Don't rub it in – let your skin absorb the moisturiser on its own.
- When the eczema is active, applying moisturiser more often (as often as you like) can help relieve the itch.
- Use after a bath or shower. Pat your skin dry and apply moisturiser while your skin is damp. Put on moisturiser within 3–5 minutes after bathing. Moisturisers are more effective if applied immediately after a bath or shower as they ‘lock in’ moisture.
- Apply all over your body, not just where there is eczema.
- Common emollients and moisturisers include fatty cream (healthE fatty cream), sorbolene + 10 % glycerine, cetomacrogol cream, paraffin (healthE paraffin 50:50 WSP:LSP), oily cream and urea cream (healthE urea 10% cream). Read more about moisturisers (emollients).
Apply steroid creams and ointments when required
Steroid creams and ointments help to reduce inflammation, making your skin less red and itchy. They are applied directly to your skin and come in several different strengths.
- Usually, you use stronger strength steroid cream (or ointment) on your body and weaker strength on your face and in skin folds. It's important to use the correct strength.
- Your doctor will tell you the correct strength to use and for how long, depending on how severe your eczema is and what part of the body it's on.
- Ask your doctor or nurse to fill in an eczema action plan(external link) so you know what cream to use where and how often.
- If you use a steroid cream or ointment for more than 2 weeks without your eczema improving, go back to your doctor as you need a different treatment.
- Read more about steroid creams and ointments.
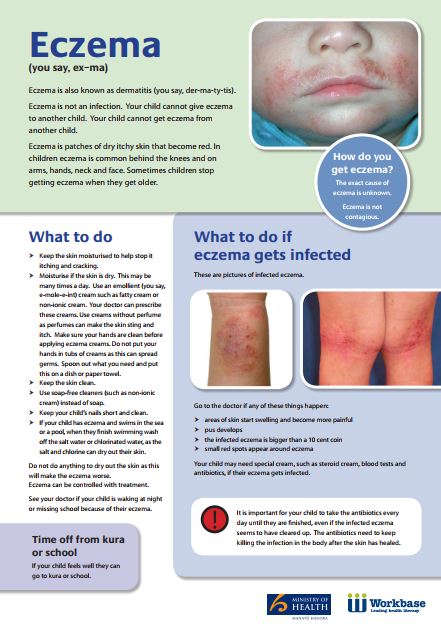
Infected eczema needs to be treated with an antibiotic. See your doctor or nurse if you have the following symptoms:
- weeping and/or crusted areas
- lots of yellow or white pimples
- sudden flaring of eczema all over the body
- shivering or fever
- skin that is painful to touch
- painful chicken pox-like blisters and sores.
- If the topical steroid does not work to make the eczema go away after 1–2 weeks.
- If eczema means school or work is missed on a regular basis.
- If eczema is affecting sleep.
- If the infection is not improving after 2–3 days of treatment or keeps coming back.
- If other people in the house have skin infections – they may also need treatment.
If you don't respond to emollients and steroids for your eczema and continue to have significant symptoms, there are other treatments that may be effective and are available by referral to a dermatologist. These include phototherapy and systemic immune modulators.
Atopic eczema(external link)(external link) DermNet, NZ
Childhood eczema(external link) KidsHealth, NZ
Eczema and allergies(external link)(external link) Allergy NZ
Bleach baths for eczema(external link) Child and Youth Eczema Clinical Network, NZ, 2023
Eczema and food – fast facts(external link)(external link) Australasian Society of Clinical Immunology and Allergy, ASCIA, 2020
Resources
Caring for your child's eczema(external link)(external link) New Zealand Child and Youth Clinical Network, 2023
Bleach bath instructions(external link) Starship, NZ, 2023
Infected eczema(external link)(external link) Diana Purvis – Paediatric Dermatologist
Eczema(external link)(external link) Health Literacy NZ
Action plans
Eczema action plan(external link)(external link) New Zealand Child & Youth Clinical Network, 2020
Caring for your child's eczema(external link) Child and Youth Clinical Network, NZ, 2020
Bleach baths for eczema (external link)Child and Youth Clinical Network, NZ, 2023
Eczema action plan(external link) Australasian Society Clinical Immunology & Allergy, 2020
Brochures
New Zealand Child & Youth Clinical Network, 2020

New Zealand Child and Youth Clinical Network, 2023
Health Literacy NZ
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Last reviewed:
Page last updated:





