Managing heart failure well needs the input of your healthcare provider who knows about your other health issues that may affect your heart failure. Other healthcare team members that may be involved in your care include a heart specialist, heart failure nurse, dietitian and pharmacist. It can also help to involve your family/whānau in your decision making.
There are also things you can do yourself to monitor and improve your symptoms. In this section you can find out about them
Have a heart failure action plan
A heart failure action plan provides you with instructions and information on how to manage your heart failure on a daily basis and also how to recognise and cope with worsening symptoms, such as flare-ups (exacerbations).
You can develop your heart failure action plan with your healthcare provider and fit the plan to suit how severe your heart failure is and your wishes. At each visit with your healthcare provider, you can review the plan and make adjustments as needed.
Here's an example of a heart failure action plan(external link) by the Heart Foundation NZ.

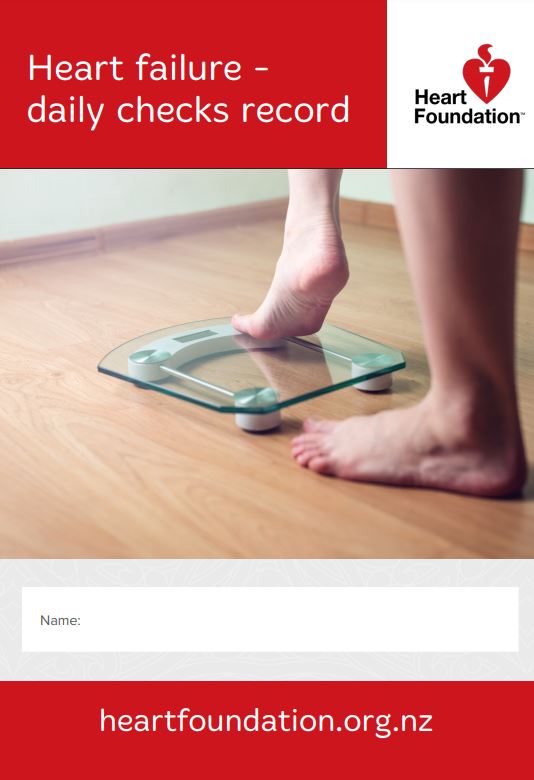
Weigh yourself each day
Your doctor may recommend you do this to check whether you have any extra fluids. If you put on more than 2kg over a few days, your body is retaining fluid, not fat. Your doctor will help you work out your target weight – this is your weight with no extra fluid, and is the weight at which your body and heart work best.
Weigh yourself every morning each day at the same time (after you have been to the toilet, before you eat or drink anything and before you get dressed). Use digital scales, and use these on a firm surface, eg, lino or tiles. Then record your weight on your heart failure action plan and remember to bring it with you to every appointment with your healthcare team.
Other than weighing yourself, you also need to check for swelling. Check whether your rings, waistband, socks or shoes feel tighter. You can also press firmly into the skin of your ankle, shin and knee with your finger. If your finger makes a dent that doesn’t quickly fill, you have swelling.
You should also monitor any changes in your breathing. If you are more short of breath than usual or have more swelling, you are likely to retain more fluid.
Follow the steps in your action plan as discussed with your healthcare team or contact your doctor if you are concerned about any aspect of your health.
Healthy eating
Choosing healthier foods, such as whole grains, smaller portions, healthy fats, low-salt and less processed foods, can help you manage your heart failure or other health issues you may have. Avoiding or limiting salt is particularly important in heart failure as salt makes you retain fluid and makes it difficult to get rid of fluid from your body. Read more about healthy eating.
Limit fluids
You should avoid having too much fluid, but you don’t need to restrict your fluids too much unless your doctor advises you to do so. Drink about the same amount each day. Remember other food may contain fluids, such as yogurts, soups, teas, ice cream or smoothies. If you are not sure how much fluid you need to have, contact your doctor.
Stop smoking
Smoking makes you even more breathless, continues to damage your heart and dramatically increases your chances of a heart attack. Ask your doctor or nurse to get support to help you quit smoking.
Limit alcohol
People with weak hearts don’t cope well with alcohol, even in moderate amounts. Drink only small amounts and don't binge drink. If your heart failure is caused by too much alcohol, you should not drink at all.
Look after your mental health
You also need to look after your mental health. You might have lots of different feelings while coping with your symptoms, such as anxiety, stress or depression.
Try to avoid stressful situations. If you get stressed, use relaxation techniques such as taking 6 slow, deep breaths. Doing something where you feel useful and gain a sense of achievement can help you regain balance in your life.
It also helps to have plenty of rest and get a good night's sleep, as this allows your body and mind to restore. Talking to family/whānau members can also help. If you need more support, ask your healthcare team for a referral to a psychologist or counsellor.
Stay active
Start exercising gently by doing a little, and slowly increase your activity as you manage more. Try walking gently around the house or down the road first. Ask your doctor or nurse about suitable exercises for you or about any exercise programmes available in your area.
Have a healthy body weight
Losing weight if you are overweight helps takes the strain off your heart and can help you feel better. If you are underweight or have a poor appetite, having foods that are higher in calories and protein, or high-energy drinks, can help boost your energy. Ask your doctor, nurse or dietitian for advice on how to reach a healthy weight.
Get vaccinated
Vaccination against the flu and pneumococcal disease is recommended as these infections can worsen your symptoms. Ask your healthcare team about getting these vaccinations, and the COVID-19 one.
Attend regular follow-ups
It is important to attend your follow-up appointments regularly. This allows your doctor or nurse to monitor your health and see how your condition is progressing, as well as review your medicines and answer any questions you may have. Bring your heart failure action plan with you so that your healthcare team can monitor and better understand what is happening for you.
Join a cardiac rehabilitation programme
You may be advised to attend a cardiac rehabilitation group at your local hospital. These are excellent for learning more about ways to strengthen your heart again and supporting you to get more active. Some local gym's also have exercise classes for people with heart failure.
Read more about cardiac rehabilitation.