Treating chronic pain is complex. Treatment usually won’t make the pain go away. Instead, the aim of treatment is to find ways to reduce the impact pain has on your life.
Commonly used pain relief medicines are a useful option for treating short-term (acute) pain, but they are not very effective in treating chronic pain and when used long term, can have more side effects. However, there are some medicines that can be used alongside physiotherapy, exercise, balanced diet, relaxation and different ways of thinking and responding to pain. Read more about reducing chronic pain – what you can do to help yourself [PDF, 210 KB].
Low or no data? Visit zero.govt.nz, scroll down the page then click on our logo to return to our site and browse for free.
Pain relief medicines for chronic pain
Key points about pain relief medicines for chronic pain
- Commonly used pain relief medicines are not very effective in treating chronic pain and when used long term, can have harmful side effects.
- Treating chronic pain is complex.
- Treatment usually won’t make the pain go away. Instead, the aim of treatment is to find ways to reduce the impact pain has on your life.

| Medication | Usefulness |
| Paracetamol | Paracetamol is used to treat mild-to-moderate pain. For some types of chronic or long-term pain, taking paracetamol at regular set times is likely to be most helpful.
|
| Antidepressants such as amitriptyline, nortriptyline |
These medicines are usually used to treat depression but low doses can be used to treat nerve pain caused by shingles, diabetes, stroke and spinal cord injury.
|
| Gabapentinoids such as gabapentin, pregabalin | Gabapentinoids can be used to treat nerve pain caused by shingles, diabetes, stroke and spinal cord injury. They help to dampen down the activity in the nerves that are irritated or damaged.
|
| Non-steroidal anti-inflammatories (NSAIDs) |
Examples include ibuprofen, diclofenac, naproxen and celecoxib. NSAIDs can be used for a short time when you have a flare-up of symptoms.
|
| Opioids |
Examples include codeine, tramadol, morphine and oxycodone. Opioids can be used to treat moderate-to-severe pain that comes on suddenly (acute pain) or for chronic pain caused by cancer.
|
If you are using medicines for chronic pain, it is a good idea to develop a pain management plan with your doctor, which can be discussed and then written down. This plan should provide you with clear guidance on how to use your medicines correctly, including:
- the dose and how often to take them
- when or if you can increase the dose
- common side effects
- how to reduce the dose and stop medicines as your pain improves.
It should also include a review schedule, such as seeing the doctor again within 2 to 4 weeks of starting a medicine or changing a dose, to see if you have any side effects and assess how well your pain is controlled.
Medicines for chronic pain(external link) Healthify He Puna Waiora, NZ and PHARMAC, NZ, 2018
Reducing chronic pain – what you can do to help yourself(external link) Healthify He Puna Waiora, NZ and PHARMAC, NZ, 2018
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
References
- The principles of managing acute pain in primary care(external link) BPAC,NZ, 2018
- Prescribing gabapentin and pregabalin: upcoming subsidy changes(external link) BPAC, NZ, 2018
- Managing patients with neuropathic pain(external link) BPAC, NZ, 2016
- Helping patients cope with chronic non-malignant pain: it's not about opioids(external link) BPAC, NZ, 2014
Brochures
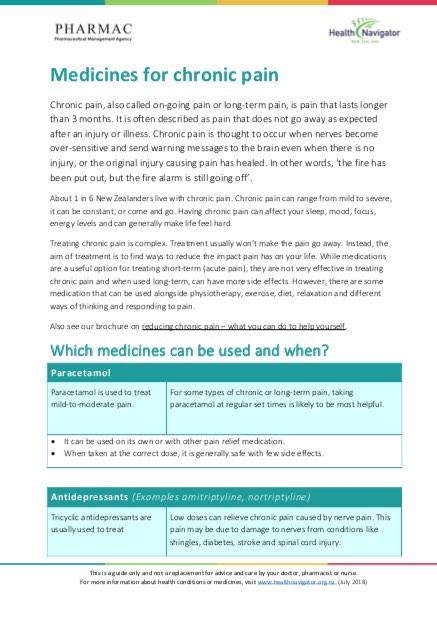
Healthify He Puna Waiora, NZ and PHARMAC, NZ, 2018
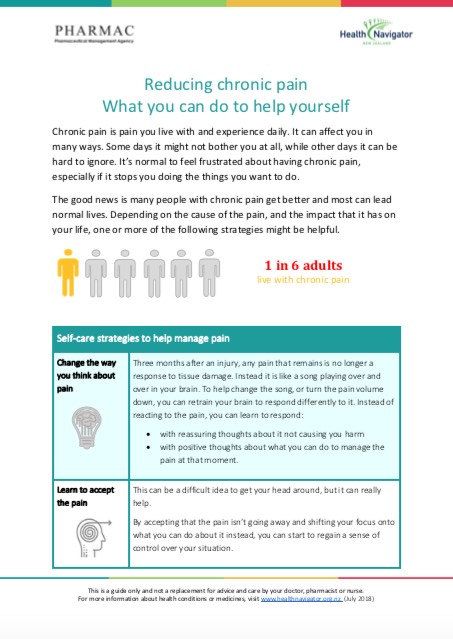
Healthify He Puna Waiora, NZ and PHARMAC, NZ, 2018
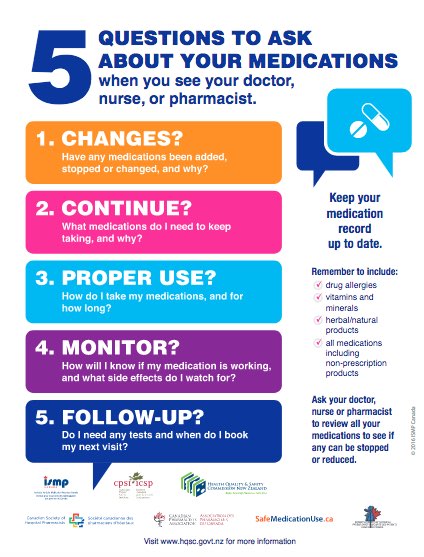
Health Quality and Safety Commission, NZ, 2019
EnglishTe reo Māori
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Page last updated:





