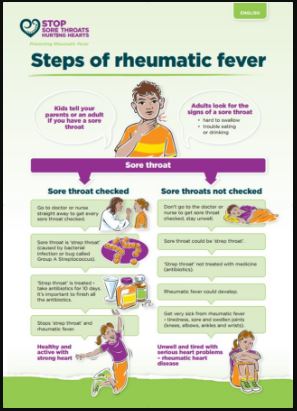
The treatment of strep throat depends on your risk of getting rheumatic fever. If you are at low risk, treatment is aimed at self-care to ease the pain and the infection will get better on its own in a few days. However, some people will also need antibiotic medicine.
Self-care
- Suck a teaspoon of honey (not safe for children under one year) or gargle salt water.
- Adults can try using a gargle, throat spray or pain-relief (anaesthetic) lozenges. These are not suitable for children.
- Take paracetamol – check doses carefully and ask your doctor or pharmacist whether it is safe for you.
Antibiotic medicine
If you have a higher risk of getting rheumatic fever, or if you have a high risk of spreading the bacteria, eg, you are a healthcare worker, residential care worker, food handler, teacher, childcare worker or student, treatment with antibiotics may be started as soon a throat swab is done.
- Antibiotics (penicillin or amoxicillin) are normally given for 10 days. You should finish the full course to make sure the strep throat does not cause rheumatic fever.
- A one-off antibiotic injection to treat a strep throat might be a good alternative for children if you think they may find it hard to take the full 10-day course of capsules or liquid.
- Keep children away from school or early childhood centres for at least 24 hours after they start antibiotics, to reduce the risk of spreading the strep bacteria.