DO
- test for COVID
- give pain relief such as paracetamol or ibuprofen
- check with a pharmacist if a throat spray or medicated lozenges are ok for your child
- drink warm liquids, eg, honey and lemon (for tamariki aged 1 year and over)
- eat cool or soft foods
- give an ice block or suck ice (if old enough)
- rest and drink plenty of fluids
- see a nurse or GP for a throat swab or antibiotics if you or your child are Māori or Pasifika aged 3 to 35 years
- allow older children to gargle with warm salt water (1 teaspoon of salt per glass of water).
DON’T
- don’t expect antibiotics as these will not help most sore throats, unless your child is high risk as above
- don’t give lozenges to young children as they might choke
- don’t send your child back to day care, kindy or school until they are well.

Image credit: Canva
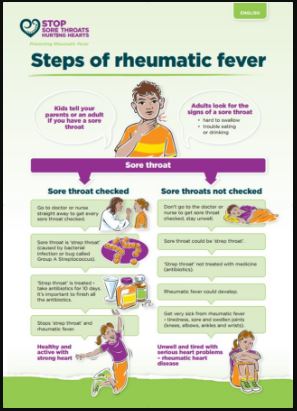
Antibiotics are only needed if your child:
- is at high risk for rheumatic fever
- has a bacterial infection and tests positive for strep throat, or they have a severe sore throat, such as with scarlet fever.
When should I see my healthcare provider?
For any of the following:
- if you or your child are Māori, or Pasifika aged 3 to 35 years
- babies under 6 months
- a sore throat and a very high temperature, or feeling hot and shivery
- a weakened immune system, eg, because of diabetes or chemotherapy
- severe pain at the back of the throat
- not able to drink much, or has a very dry mouth, or no pee (urine/mimi) for more than 8 hours
- symptoms that aren’t improving after 48 hours
- development of a rash
- fever of 38°C or above for more than 5 days
- symptoms getting worse or if you are worried
- they often get sore throats
- increased snoring or periods of stopping breathing when asleep.
When should I seek urgent help?
Call 111 and ask for an ambulance or go to the nearest hospital if your child:
- has difficulty breathing, eg, is struggling for breath or making a grunting noise with each breath
- has difficulty swallowing their own saliva – drooling can indicate this
- is confused or drowsy
- has any other symptoms that appear life-threatening.