 Source: Muscular Dystrophy Association of New Zealand, 2016
Source: Muscular Dystrophy Association of New Zealand, 2016
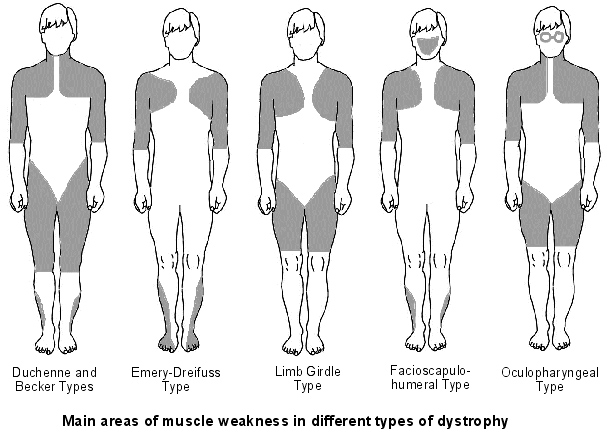
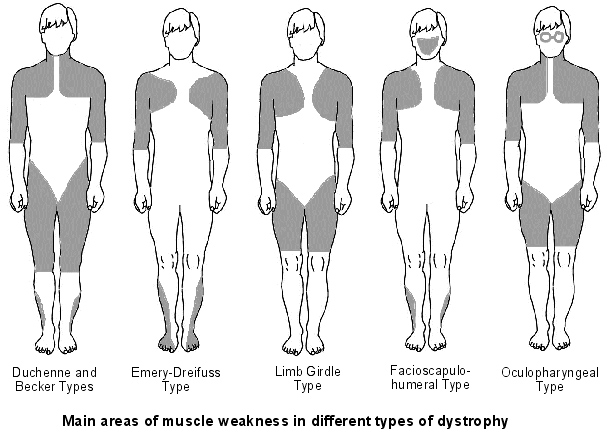
There are several recognised types of muscular dystrophy (MD). These are described below.
Duchenne muscular dystrophy (DMD)
DMD is the most common of the muscular dystrophies. It affects about 1 out of every 3,600 baby boys born. DMD is characterised by progressive difficulty in walking and performing everyday activities. The symptoms usually appear before the age of 6 and may appear as early as infancy. Typically, the first noticeable symptom is a delay of motor milestones, including sitting and standing independently. Find out more about DMD(external link).
Becker muscular dystrophy (BMD)
BMD is considered to be a milder form of DMD, as both are caused by mutations in the same gene and have similar symptoms. BMD has a later onset and slower progression. BMD occurs in about 1 in 30,000 live male births. Find out more about BMD(external link).
Manifesting carriers
A manifesting carrier is a female who displays symptoms of a condition that usually only affects males, such as BMD and DMD. Although it is a commonly held belief that carriers merely pass on the disease and are unaffected, female carriers can have similar muscular weakness as affected males. This condition can occur with no known family history of BMD or DMD, so all females who are suspected of having any form of muscular dystrophy should be tested to determine if they could be a manifesting carrier because of the genetic implications. Find out more about manifesting carriers(external link).
Congenital muscular dystrophy (CMD)
CMD causes muscle weakness within the first six months of life. It is rare, affecting about 1 in 50,000 babies and both males and females are equally likely to have this condition. Find out more about CMD(external link).
Emery-Dreifuss muscular dystrophy (EDMD)
EDMD mainly affects muscles used for movement (skeletal muscles) and heart (cardiac) muscle. It affects males and females with first symptoms usually occurring between the ages of 17 and 40. Early symptoms include joint deformities called contractures, which restrict the movement of certain joints, especially elbows, ankles and neck. Find out more about EDMD(external link).
Facioscapulohumeral dystrophy (FSH)
FSH is the third most common muscular dystrophy. It affects about 1 in 20,000 people of Caucasian origin. In FSH the muscles typically affected are those of the face, shoulder blades and upper arms. Find out more about FSH(external link).
Limb girdle muscular dystrophy (LGMD)
LGMD affects the voluntary muscles of the hip and shoulder areas, called the limb girdles. These muscles weaken and waste away (atrophy) and may involve other muscles over time. The onset of LGMD can occur in childhood or symptoms may not be apparent until adolescence or adulthood. Males and females are equally affected. Find out more about LGMD(external link).
Myotonic dystrophy (DM)
Because the Latin name is Dystrophia Myotonica, this condition is known as DM. It is a multi-systemic disorder, which means that the effects are not limited to the voluntary muscle system, but can also affect tissues and organs throughout the body. DM affects both males and females and the age of onset can be from birth to old age. It is a rare condition with three different types, of which two affects about 1 in 8,000 people and the third only 1 in 100,000. Find out more about DM(external link).
Oculopharyngeal muscular dystrophy (OPMD)
OPMD is an inherited condition that appears in early middle age. Progressive drooping of eyelids and weakness of muscles around the eyes is the first symptom, followed by difficulty swallowing food. Find out more about OPMD.(external link)



 Source: Muscular Dystrophy Association of New Zealand, 2016
Source: Muscular Dystrophy Association of New Zealand, 2016


