There are 2 types of bronchitis: acute and chronic.
This page covers acute bronchitis (chest infection) in adults. For information on chronic bronchitis (chronic obstructive pulmonary disease or COPD) see COPD. For information on chest infection in babies and children under 2 years of age see bronchiolitis.
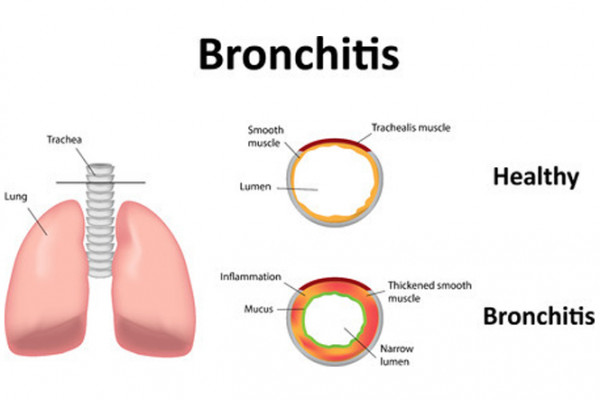
Image credit: 123rf
What causes acute bronchitis?
The main cause of acute bronchitis is a virus. This is often the same virus that causes a common cold, which is why bronchitis often occurs after a cold. Acute bronchitis is more common in winter.
Acute bronchitis can affect people of all ages. For information on chest infection in babies under 6 months of age see bronchiolitis.
What are the symptoms of acute bronchitis?
The main symptom is a chesty cough, with green or yellow mucous. You may also get cold symptoms, such as:
- mild fever
- sore throat
- aches and pains
- runny nose
- headache
- tiredness.
You’ll usually start to feel better after a few days, but the cough may remain for a few weeks.
If you or a family member is short of breath, coughing up blood, has a high fever or feels very unwell you need to see your doctor or call Healthline on 0800 611 116 straight away. These are the signs that a chest infection is more serious — it could be pneumonia or other serious conditions.