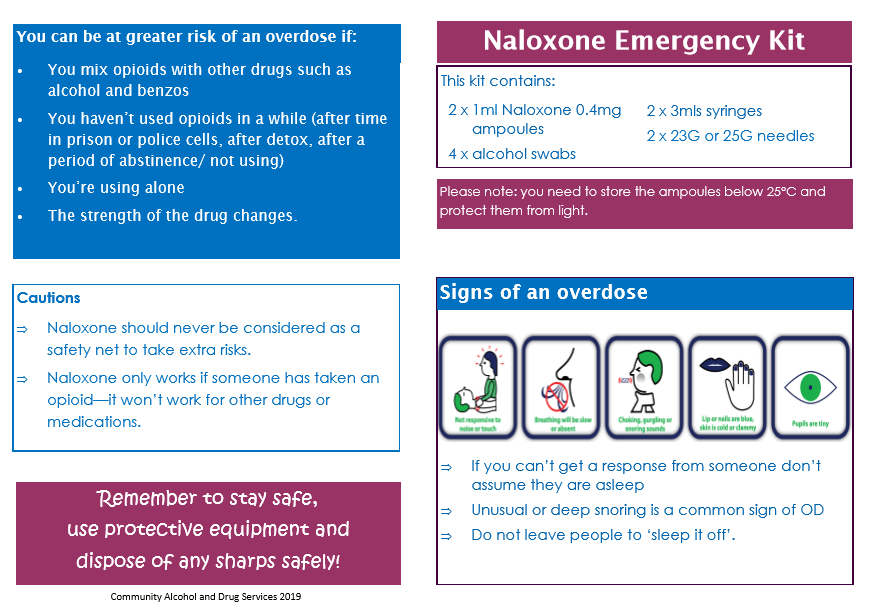
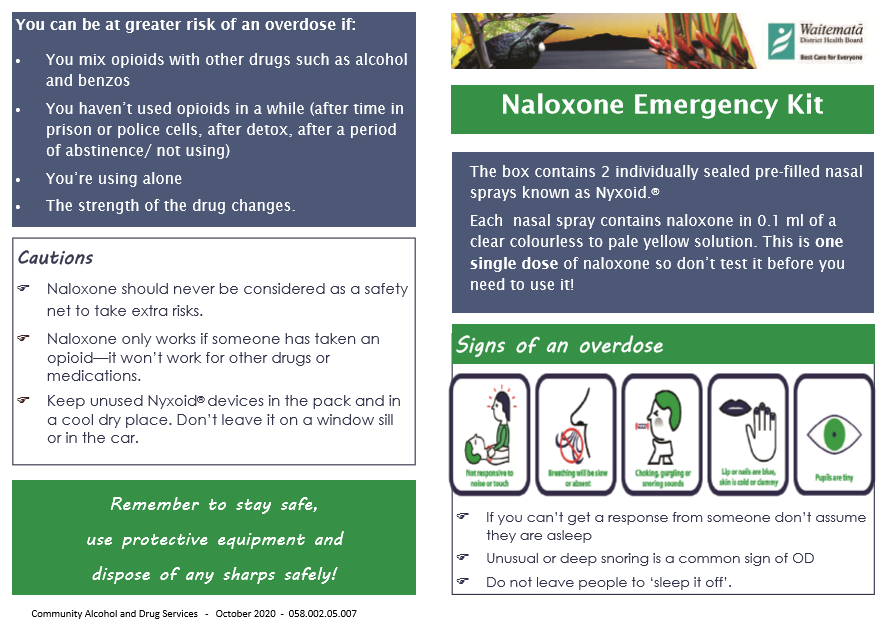
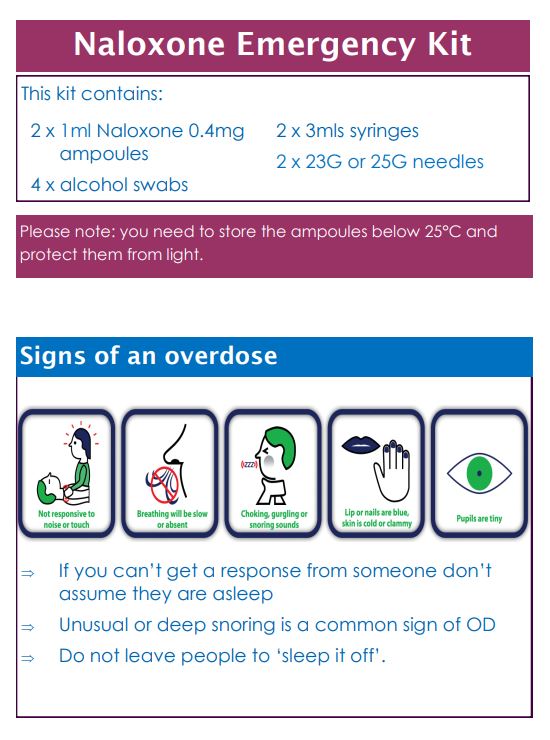
Naloxone is a medicine used to treat opioid overdose. Opioids are strong pain medicines, and drugs such as heroin. Examples of opioids include codeine, morphine, oxycodone, methadone, fentanyl, tramadol and heroin. Opioids slow your breathing and affect your consciousness – if you take too much or overdose on opioids, your breathing may stop and you could die. Read more about opioids and who is at risk of opioid overdose.
Naloxone works by reversing the effects of opioids. It can return normal breathing patterns to a person whose breathing has shallowed or stopped because of an opioid overdose. Naloxone can be given by injection or nasal spray and works very quickly, within 2–5 minutes.
| Opioid overdose is an emergency because it causes life-threatening problems such as slow or stopped breathing and unconsciousness. |