Choose your lead maternity carer (LMC)
As soon as your pregnancy is confirmed you need to choose a lead maternity carer or LMC. It's good to get onto this early. Your LMC is responsible for your care throughout your pregnancy, during labour and birth and for the first 4 to 6 weeks of parenthood.
An LMC is generally a self-employed midwife, a hospital employed midwife or a private obstetrician (a doctor who specialises in pregnancy and childbirth). A few family doctors (GPs) may also offer maternity care.
Maternity care is free for most people in Aotearoa New Zealand, however there is generally a cost for a private obstetrician or a family doctor. Find out more about who is eligible for free or subsidised maternity care(external link).
You can also visit the Find Your Midwife website(external link) which lists contact details for qualified midwives who are members of the NZ College of Midwives. There's a form to contact them directly through the website. If you can't find a midwife you can search Healthpoint(external link), just type in your address to search for a midwife in your region.
Health tests and screening
When you first see your midwife, family doctor or specialist doctor during pregnancy, you'll be offered some blood tests. These are free and are used to check:
Read more about antenatal blood tests.
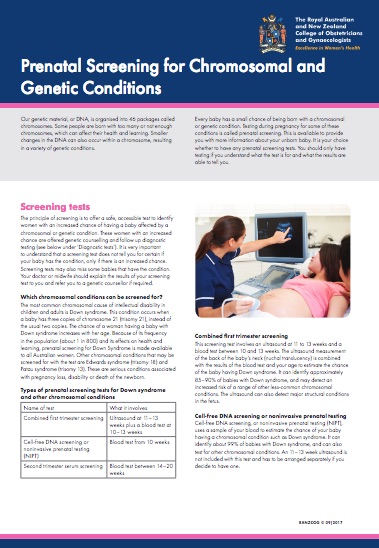
An optional test is antenatal screening for Down syndrome and other conditions, known as MSS1 or MSS2. This screening includes a free blood test and a scan that you may have to pay for. There's also another paid option known as the NIPT or non-invasive prenatal testing which screens for Down syndrome, Edwards syndrome and Patau syndrome.
If you're over 25 years of age and have never had a cervical screening test, it's important to get this done. You can now choose to do your own vaginal swab in private at your healthcare provider's clinic.
For many pregnant people a dating scan isn't necessary to work out your due date and how many weeks pregnant you currently are. It will only be offered if you're not sure of the date of your last menstrual period. Read more about pregnancy screening tests and checks.
Be aware of red flag symptoms
Any of these symptoms could be a sign that something is wrong with your pregnancy. Don't wait for your regular prenatal visit to talk about any of these. Call your LMC right away if you experience:
- severe abdominal pain or cramps
- severe nausea (feeling sick) or vomiting (being sick)
- bleeding
- severe dizziness
- pain or burning during urination (peeing).
Learn about labour, birth and looking after a baby
Many pregnant people, especially those expecting their first baby, go to classes or hapūtanga wānanga to learn more about pregnancy, giving birth and parenting. Hapūtanga wānanga is kaupapa Māori education that will also cover matauranga Māori concepts on parenting and birthing as well as Rongoā Māori.
These classes also provide an opportunity to meet other expectant parents – many groups go on to have regular catch-ups after their babies are born.
Talk to your LMC about the classes and wānanga that are available in your area. Most hospitals provide a limited number of free classes. There are also privately run classes as well as online options – you usually have to pay for these.
Find out about parental leave
You can get up to 10 days unpaid special leave while you're pregnant. This is for medical appointments, antenatal classes etc and doesn't have to be taken as a full day's leave. Find out what paid and unpaid parental leave you're entitled to and how to apply for it at types of parental leave(external link).
Staying healthy in the first trimester
The first trimester is vital for the development of your baby. Your baby will develop all of its organs by the end of the third month. To stay healthy and support this growth read about: