The majority of healthcare services are funded by the Ministry of Health – a government department. The Ministry of Health provides the bulk of its funding for health services to District Health Boards (DHBs), who in turn divvy up the money between what’s called primary and secondary care.
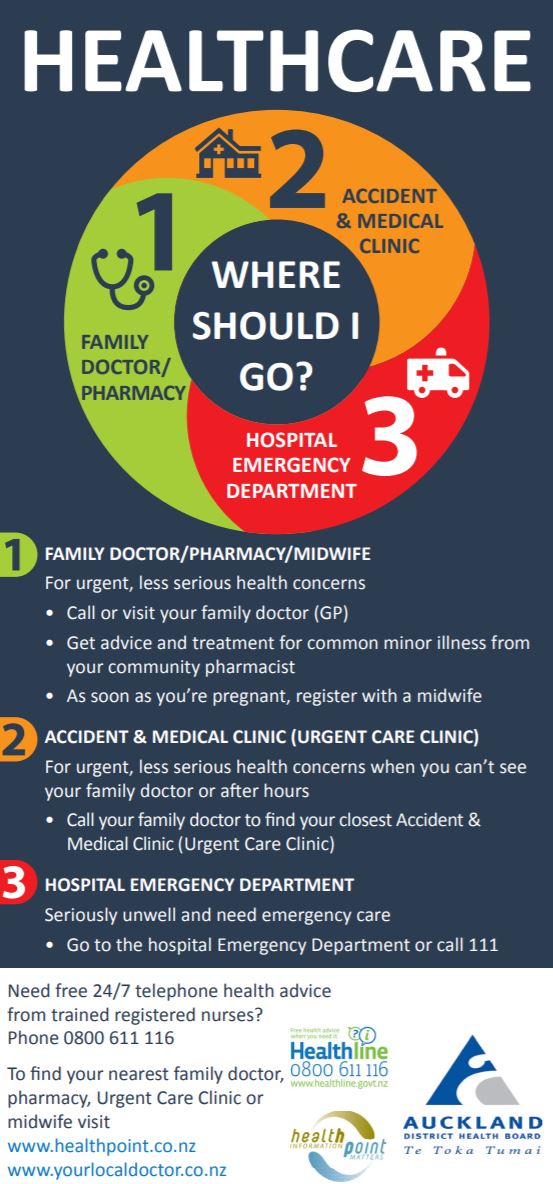
Services you would encounter in primary care include contact with your family doctor or GP, practice nurse, midwife, Plunket nurse, physiotherapist or podiatrist.
Many of these services are funded, but the funding doesn’t always meet all the cost of providing the service by these private businesses. This means you may be charged what’s called a co-payment or fee for some of these services.
What are primary care services?
Funding for primary care comes from District Health Boards and goes to Primary Health Organisations (PHOs). PHOs are generally charitable trusts and exist in a single area, for example the North Shore of Auckland.
For GP clinics to access the Government funding, they must become a member of a PHO. The amount of funding a PHO and its member GP clinics receive is based on how many patients and the health needs of the people registered. For example, more funding is provided for people living in low socio-economic areas and those with chronic illness like diabetes, asthma or heart disease.
What are secondary care services?
Secondary care services generally include any contact with the hospital – an appointment, visiting the emergency department, surgery or assistance with maintaining your health if you have a chronic illness, like diabetes or kidney disease where you might need regular visits to the hospital for dialysis.
All these services are fully subsidised, or free for New Zealanders.
What about private hospitals?
Private hospital care is available in New Zealand, but at a cost. Generally, only people with insurance or the ability to pay will use a private hospital for procedures, diagnostic tests and surgery.
Many procedures done in a private hospital can also be done in a public hospital, but the difference is there may be a wait of several weeks or months. Care in some private hospitals, for example in rest homes or aged care facilities, are subsidised.