Usually people with mild forms of vWD do not require special medicines unless they have surgery, dental work or an accident or injury. If you have a bleed, applying pressure to the wound (or pinching the soft part of your nose if you have a nosebleed) for a few minutes may be all you need to do.
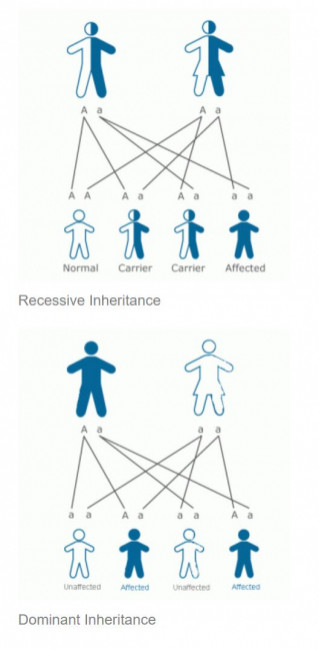
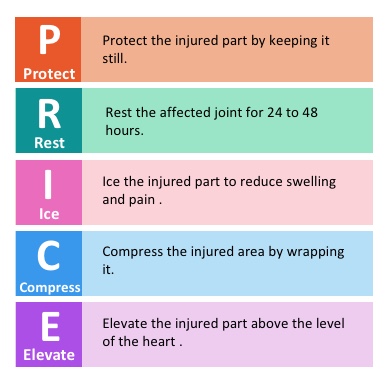
Minor bleeding problems like bruising can be managed with the PRICE approach (protect, rest, ice, compression and elevation).
Using PRICE to treat bleeds
Mild bleeds can be managed with the PRICE approach – protect, rest, ice, compress and elevate.
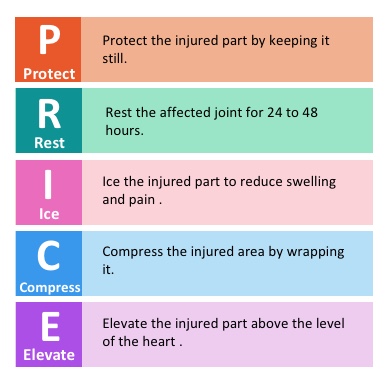
Protect
Reduce weight bearing or stress on the affected joint or muscle by using crutches or other supports such as a 'collar and cuff' for the arm.
You may need to avoid putting weight on the affected side completely for the first 48 hours and possibly longer if it is a severe bleed.
Rest
The affected area should initially be rested completely, generally for the first 24–48 hours depending on the severity of the bleeding episode. This allows the swelling to go down and prevents further bleeding.
The injured area should not be forced into any position, but instead rested in the most comfortable position possible. Remember, rest is not the same as immobility, as too much rest can also be damaging, so start to move the joint gently, as pain allows, within one or two days of treatment.
Ice
Ice helps to reduce swelling, prevent further bleeding and eases pain.
- Use a gel cold pack or a CryoCuff if you have one.
- If not, make an ice pack from a bag of frozen peas or crushed ice wrapped in a cloth.
- Cold wraps or packs should be applied to the affected area little and often for around 10–15 minutes every 2 hours or so.
- You may need to continue using ice for several days after the bleed if your joint is still warm and swollen.
- Do not apply for more than 20 minutes at a time and do not place ice directly on the skin as it can burn.
Compress
The more swollen a joint or muscle becomes, the more pain you will feel. Compression reduces swelling and therefore pain. If the muscle or joint is very swollen, you may need to wait a day or so before using a compression bandage and then apply as pain allows.
Your nurse or physiotherapist can provide you with an elasticated bandage and will make sure it fits correctly, as additional damage can be caused where the bandage is too tight.
Try not to allow wrinkles in the bandage and make sure to remove it at night before you go to sleep.
Elevate
This helps to reduce swelling and relieve pain by increasing the blood flow away from the injured area.
- The injured area should be raised above the level of your heart.
- When you elevate your leg, remove the compression stocking to allow normal, healthy circulation.
- Elevate little and often for around 20 minutes at a time.
Using medicine to treat bleeds
Your doctor may also give you medicine to help stop bleeding when it happens.
The three main medicines that can help stop bleeds are tranexamic acid, desmopressin and concentrated von Willebrand factor.
Tranexamic acid
- This can be used to stop bleeding in your mouth or for nosebleeds, gut bleeding, bleeding after dental work, minor surgery or an injury.
- Tranexamic acid works by maintaining a clot (preventing a clot from dissolving once it has formed) – it does not help form a clot.
- It is most commonly taken as tablets, but may also be used as a mouthwash.
- Read more about tranexamic acid
Desmopressin
- Desmopressin is usually used for more serious bleeds. It copies a natural hormone in your body that acts by releasing von Willebrand factor stored in the lining of your blood vessels and helps blood to clot.
- Desmopressin is not suitable for everyone – people react to desmopressin in different ways and your doctor will need to test your response to desmopressin to check whether it will work for you.
- It can be given as a slow injection into a vein, but may also be given as an injection into the fatty tissue under your skin (subcutaneously) or, in special circumstances, as a nasal spray.
- Since von Willebrand factor stores in your blood vessels are limited, you may need to wait for your body to rebuild its stores of VWF before taking another dose, usually about 24 hours.
- Desmopressin can also have mild side effects such as facial flushing, headache, feeling sick (nausea) and water retention.
Concentrated von Willebrand factor
- Clotting factor concentrate made with von Willebrand factor (VWF) and factor VIII (FVIII) replaces the missing VWF and FVIII in your blood and helps blood to clot.
- This clotting factor concentrate is made from the plasma (pale yellow fluid part) in human blood and is produced from blood donations.
- Clotting factor concentrate is used when desmopressin is not suitable, or when it is likely you will need treatment for more than 2–3 days, such as after major surgery.
- The treatment is infused (injected) into a vein in your arm.
Treatments for heavy periods
If you have heavy periods as a result of vWD, speak to your GP or specialist about treatments to help control the bleeding.
As well as the medicines above, birth control pills (oral contraceptives) or other hormone treatment may be prescribed. They help to increase vWF and Factor VIII levels and control menstrual bleeding.