A macular hole can be treated and repaired with surgery called a vitrectomy. The surgery is usually done as a day (outpatient) surgery and there is a greater than 95% success rate. There is no other treatment for a macular hole.
During a vitrectomy:
- You will be given medicine to help you relax and your eye will be numbed to dull the pain (anaesthesia).
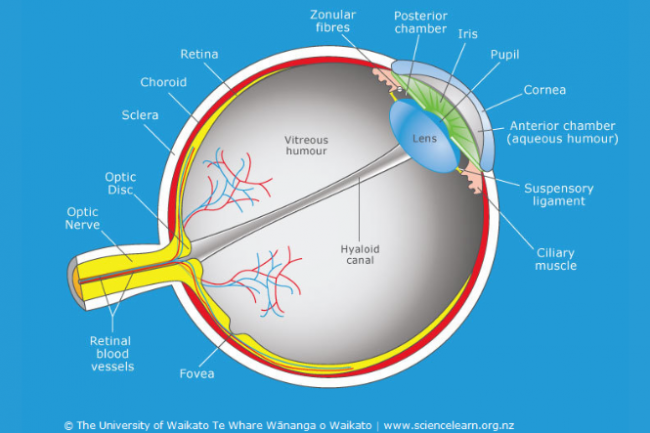
- The surgeon will make very small holes through the white part of the eye.
- These holes are so small that usually no stitches are required.
- Using a microscope, the surgeon can use a variety of very specialised instruments placed through these holes to work within the eye.
- The gel-like substance that fills the eye is removed and replaced with a specially designed saline solution.
- The surgeon then peels a very thin membrane from the surface of the macula surrounding the macular hole.
- Peeling this membrane is important for helping the macular hole to seal.
- Finally, a gas bubble that completely fills the back of the eye is used to replace the saline solution.
- The gas bubble will gradually go away after surgery and is replaced by the gel-like fluid that is produced normally inside the eye.
- Laser and freezing treatment may also be used to secure the retina in place.
Care after surgery
- A patch is worn over the eye until the morning after surgery.
- Eye drops that help healing are used several times each day for four weeks after surgery.
- People are usually asked to position themselves face down for five days immediately following the operation. Positioning face down allows the gas bubble to press firmly against the macular hole and may slightly increase the chance of the hole closing well. Your eye specialist will discuss this with you.
Outcomes of surgery
Usually, vision recovers to ‘normal’ (6/6) or to the vision required for a driver's licence (6/12) after successful macular hole surgery. However, some people may have more limited improvement in vision and a small percentage of people may not improve very much at all even after successful surgery.
The amount of visual improvement depends on:
- whether the macular hole closes
- the person's age
- the physical condition of the macular hole
- other existing eye problems.
After the surgery it can take anywhere from 3–18 months for your vision in the affected eye to reach its best.
Possible complications of macular hole surgery
Any surgical procedure carries a risk of complications and macular hole surgery is no exception. There are 3 main complications of macular hole surgery to be aware of:
Infection of the eye after surgery: Most infections can be effectively treated if picked up at an early stage. However, there is a risk that an infection can create severe damage that could lead to blindness in the affected eye. Fortunately, eye infections after surgery are rare, occurring in only 1 of 2000 cases.
Retinal detachment: This can occur at any time, even if there has been no surgery. However, if you have had macular hole surgery, your eye is at greater risk of developing retinal detachment. A retinal detachment can occur soon after surgery, and occasionally it can develop months or years later. It can lead to blindness if not repaired. Fortunately, nearly all retinal detachments can be repaired with additional surgery. Retinal detachment after macular hole surgery occurs for 1 or 2 out of every 100 people. Ongoing improvements in surgical techniques and instruments are reducing this likelihood.
Cataracts: These cause haziness in the lens of the eye and commonly develop as a natural consequence of ageing. Having a vitrectomy causes cataracts to progress more quickly. Cataract surgery may be needed within 1 year of vitrectomy surgery.