- Gastroenteritis is a bowel infection causing diarrhoea, and sometimes vomiting.
- Diarrhoea means runny, watery poo.
- Children need to drink plenty of fluids if they have gastro.
- Give small amounts of fluid often.
- Gastro can cause dehydration, especially in babies and young children.
- Watch for signs of dehydration (such as dry lips, fewer wet nappies, sunken eyes, unusual sleepiness) and contact your doctor urgently if you suspect it.
- If your baby is less than 6 months old and has vomiting and/or diarrhoea you should contact your doctor urgently - babies can become dehydrated and unwell quickly.
Low or no data? Visit zero.govt.nz, scroll down the page then click on our logo to return to our site and browse for free.
Gastroenteritis in children
Key points about gastroenteritis in children
- Gastroenteritis (gastro) is a bowel infection, usually caused by a virus.
- It causes runny, watery poo (hamuti) and sometimes vomiting. Children with gastroenteritis need to drink plenty of fluids.
- If your baby is less than 6 months old and has vomiting or diarrhoea you should contact your doctor urgently. Babies can become dehydrated quickly.

A virus usually causes gastro. Common viruses are rotavirus and adenovirus but there are many others. Because there are many viruses that cause it, your child can get gastro more than once.
Infants younger than 15 weeks of age can have rotavirus immunisation free of charge. This protects against one of the most common causes of gastro. Read about rotavirus immunisation.
Sometimes bacteria can cause gastro but this is much less common. This can cause blood in the poo.
A child can catch the virus when they:
- touch something which has been in contact with the diarrhoea or vomit of a person with the infection, and
- they put their hand in their mouth.
The virus is easily spread in homes, day care, kindergartens and schools.
The vomiting may settle quickly but the diarrhoea often lasts for up to 10 days. This doesn't matter as long as your child is drinking well and seems to be improving.
Gastro affects all age groups, but is more common, and can be worse, in babies and young children.
The most common symptoms are:
- feeling sick (nausea)
- diarrhoea (runny, watery poo)
- vomiting
Sometimes a child with gastro will also have:
- a fever
- tummy pains

Image credit: Canva
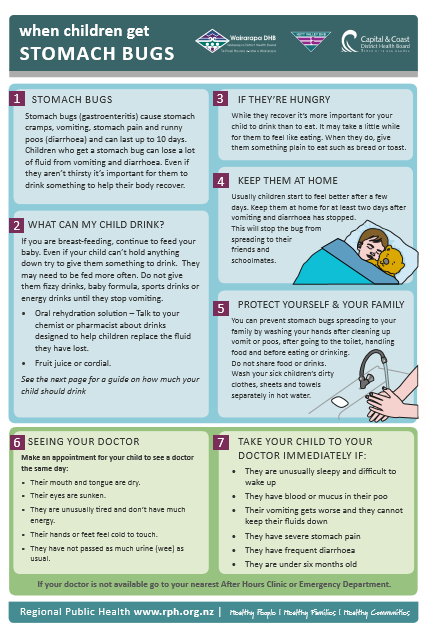
If your child is over 6 months old and has mild gastro and is not dehydrated, you can care for them at home. The main treatment is to keep giving your child fluids. Whichever fluids your child is having, the important thing is to:
- Offer small amounts of fluid often rather than giving large amounts – aim for a quarter of a cup every 15 minutes or 1 teaspoon or 5 mLs in a syringe every minute.
- Keep offering your child fluids even if they are vomiting.
Types of fluids
- If you are breastfeeding, continue to feed on demand - you may need to feed more frequently and take extra fluid.
- If your child is on formula, continue to give them formula feeds.
- If your child is over 1 year, you may give them cow's milk.
You may also give your child the following drinks as long as they are not dehydrated. You need to dilute the drinks with water as they contain too much sugar (which can make the diarrhoea worse).
- Apple juice – mix 1 part juice to 1 part water.
- Cordial – make up to normal drinking strength then add 1 part of water to 1 part of made up cordial.
- Soup – add 1 part of water to 1 part of soup.
- Fizzy drinks such as lemonade – add 1 part of warm water to 1 part of drink (warm water removes the bubbles).
Your doctor or pharmacist may recommend electrolyte solutions such as Gastrolyte or Pedialyte if your child is dehydrated. You can buy these from your pharmacist – follow the instructions on the packet. Read about electrolyte solutions (also called oral rehydration solution).
Do not give infants or children/tamariki with diarrhoea:
- undiluted soft drinks, fruit juices, Lucozade, Ribena, sports drinks (such as Powerade or Gatorade) – these contain too much sugar and can make your child's diarrhoea worse
- coffee and tea – these can make your child dehydrated.
- You can offer your child food if they are hungry, even if diarrhoea continues.
- Continuing to feed your child can speed up recovery and can reduce the length of time your child has diarrhoea.
- Your child may refuse food at first - this is not a problem as long as they take fluids.
- If possible, do not stop giving food for more than 24 hours.
- Starchy simple foods are best - try and offer foods such as bread or toast, porridge, rice, potatoes, plain biscuits, yoghurt, milk pudding.
Do not give your child fatty or sugary foods such as:
- takeaways
- chippies, sweets, cakes, chocolate, ice cream, cream, coconut cream.
Do not give your child medicines to reduce diarrhoea. They do not work and may be harmful.
Your doctor may occasionally prescribe a medicine for vomiting. Follow your doctor's instructions.
You can't treat viral gastro with antibiotics. The body will clear out the virus on its own without treatment.
Diarrhoea can cause a rash. After each bowel motion, wash and dry your child's bottom well and then put on a protective cream or ointment (such as zinc and castor oil cream or Vaseline).
Watch for signs of dehydration – the younger the child, the easier it is for them to become dehydrated.
Dehydration is the loss of fluid, due to vomiting and diarrhoea. The younger the child, the easier it is for them to become dehydrated.
Watch for signs of dehydration:
- Dry mouth and tongue.
- Sunken eyes.
- Cold hands and feet.
- Unusual sleepiness or lack of energy.
- Fewer wet nappies or not passing as much urine as usual.
If your child has any of these signs, you need to contact a doctor urgently.
You should contact your doctor or after hours medical centre urgently if:
- Your child has vomiting and/or diarrhoea and is less than 6 months old – babies can become dehydrated and unwell quickly.
- Your child is drowsy and difficult to rouse.
- Your child has a lot of diarrhoea (8 to 10 watery motions in 1 day).
- There is blood or mucus in your child's poo.
- Vomiting is increasing or your child cannot keep fluids down.
- Your child starts vomiting green fluid (bile).
- Your child develops severe stomach pains.
- Your child shows signs of dehydration.
- You are concerned for any other reason.
You should contact your doctor if your child's diarrhoea continues for more than 10 days.
Dial 111 within Aotearoa New Zealand for urgent medical help (use the appropriate emergency number in other countries) if you are very concerned about your child.
Gastro spreads very easily to others. There are ways to help prevent spreading the disease.
Thorough handwashing
Handwashing is especially important after going to the toilet, after nappy changing and before handling food. Encourage your child to wash and dry their hands after using the toilet.
Cleaning toilet and bathroom areas
It is a good idea to thoroughly clean your toilet and bathroom areas.
Washing dirty clothes
Wash your child's dirty clothing, in hot water preferably, and rinse separately from the rest of the family laundry.
Avoiding sharing food and drinks
Make sure your child doesn't share food or drinks with anyone else.
Keep them away from others
Keep your child away from friends and other children until vomiting and diarrhoea have stopped. Children with diarrhoea must stay away from day care, kindergarten and school until there has been no diarrhoea for 48 hours.
Gastroenteritis(external link) Kidshealth, NZ
Rotavirus(external link) Immunisation Advisory Centre, NZ
Resources
Viral gastroenteritis(external link) Regional Public Health, 2017
Gastro factsheet [PDF, 377 KB] Wairarapa DHB, Hutt Valley DHB, Capital & Coast DHB, NZ
Preventing dehydration in unwell children [PDF, 192 KB] Healthify He Puna Waiora, NZ, 2022
Brochures
Regional Public Health, 2017
Wairarapa DHB, Hutt Valley DHB, Capital & Coast DHB, NZ
Healthify He Puna Waiora, NZ, 2022
Credits: Content shared between HealthInfo Canterbury, KidsHealth and Healthify He Puna Waiora as part of a National Health Content Hub Collaborative.
Last reviewed:
Page last updated:





