SMILE: Self-Management is Life Enhancing Project
The vision for SMILE is to normalise self-management support in ProCare-affiliated practices in the Manukau locality. As part of this project, in 2016, ProCare worked in collaboration with the Mt Wellington Family Health Centre to pilot the health coach model.
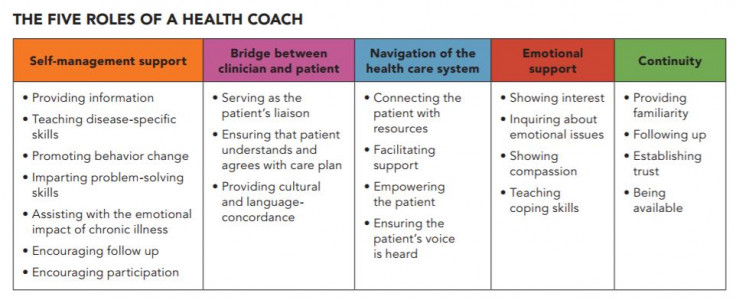
This pilot enabled the SMILE team to identify the skills and competencies for the health coaching role and develop a job description for use by other general practices. They also identified the issues that patients covered in their health conversation topics.
The most frequent topic was appointment booking, followed by goal setting, healthy lifestyle, nutrition and whakawhanaunga (nurturing the relationship). Other issues included blood glucose levels and medication.
Source: Manaaki Hauora Supporting Wellness Campaign report,(external link) Ko Awatea, Counties Manukau DHB
Health coaching workshops
As part of its Kia Kaha project, Manage Better Together, Ko Awatea runs training in health coaching. The project is part of its Manaaki Hauora – Supporting Wellness campaign, which aims to help people with long-term conditions manage their own health for a better life.
The original Kia Kaha was developed as a model of care in the primary care setting for people living with two or more long-term conditions who require significant levels of hospital-based care. It has now expanded the original team to include options for self-management education, health psychology, peer support and care co-ordination.
This has led to running two-day health coaching workshops, which have been attended by primary and secondary care health workers, including diabetes specialists, pharmacists, nutritionists, psychologists, peer workers and volunteers.
Organiser and health psychologist Leona Didsbury says, “We’re very encouraged about the value of health coaching skills as an enhancement of practice for anyone working with patients as it is very patient-centred. We are especially excited about the possibilities of health coaching ‘teamlets’ working together in primary care. Our feedback to date indicates people find this training relevant and useful for their setting.”
East Tamaki Healthcare (ETH) PHO health coaching programme
Building on the success of their peer-led self-management education (SME) programme, Kia Kaha, ETH has initiated a health coaching programme. It has also expanded the original team to include options for self-management education, health psychology, peer support and care coordination.
To support the development of health coaches within their team, they have also been running two-day health coaching workshops as part of the Manaaki Hauora project. These workshops have been attended by primary and secondary care health workers, including diabetes specialists, pharmacists, nutritionists, psychologists, peer workers and volunteers.
Organiser and health psychologist Leona Didsbury says, “We’re very encouraged about the value of health coaching skills as an enhancement of practice for anyone working with patients as it is very patient-centred. We are especially excited about the possibilities of health coaching ‘teamlets’ working together in primary care. Our feedback to date indicates people find this training relevant and useful for their setting.”
Leona is a trained facilitator of the University of California's Centre for Excellence in Primary Care health coaching programme. She has run several training sessions as this is proving to be a popular course for both regulated and non-regulated health staff, both from ETH and other organisations in the Counties Manukau district.
All health coaches working in ETH have regular supervision as well as a weekly mentoring and support session. The health coaches reflect the cultural and linguistic makeup of the enrolled population.
Challenges have included getting the resources to do the training and quality control, the need to maintain and support the lay and volunteer workforce, and referral of patients to the programme.
To overcome these challenges, support from Counties Manukau Health and Ko Awatea as part of the Manaaki Hauora campaign has made a big difference, as well as the seed funding that enabled it to happen. A validated and structured health coaching model has enabled role definition boundaries.
Key lessons that may be useful for other teams who are interested in starting health coaching include to:
- build on what works (lessons from the SME implementation informed the model)
- apply the improvement science methodology rather than depend on evidence from RCTs
- give time to explore ideas and to change and do things differently
- use a structured health coaching programme because it makes the idea easier to sell to others in the organisation, particularly clinical staff
- include information about the programme in in-house online publications
- offer a menu of options.
The model below shows how health coaching fits into the overall SME approach.

(Source: East Tamaki Healthcare (ETH) PHO – Health Coaching Programme)