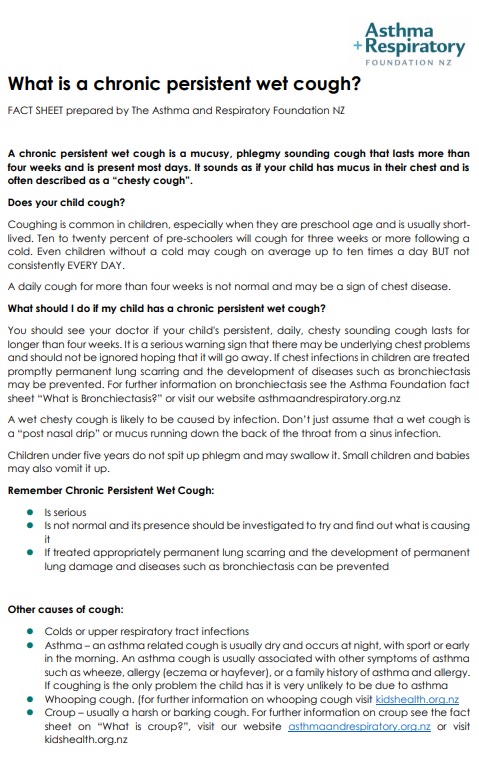
There are no medicines to treat most coughs. Antibiotics don’t help a cough caused by a viral infection. They are only needed if your doctor finds that your child's cough is due to a bacterial infection in their throat or chest.
Image credit: Canva
Self-care can help to relieve symptoms and make your child more comfortable
- Encourage rest and give lots of water to drink.
- For children older than 12 months, honey can help soothe their cough.
- Vapour rubs can be applied to their chest and back. However, there is little scientific evidence as to how well they work and they are not recommended for babies under 3 months. Avoid putting the rub near the nostril area.
- Simple pain relievers such as paracetamol (commonly known as Pamol or Panadol) can be used to reduce pain or fever and make your child more comfortable. If you aren't sure how much to give, use our paracetamol dose calculator.
- Cough and cold medicines are designed to help reduce the symptoms of the common cold such as runny nose and cough. They do not cure the infection. The ingredients in these medicines can cause serious side effects in young children. To avoid harm:
- over-the-counter cough and cold medicines are not recommended for children under 6 years of age
- only those labelled as safe for children should be given to children 6 years of age and older.
- find out more by talking to your pharmacist or see cough and cold medicines – advice for parents.
- Keeping your home smoke free, warm, clean and dry is best for your children’s health. Read more about keeping your home warm and dry.