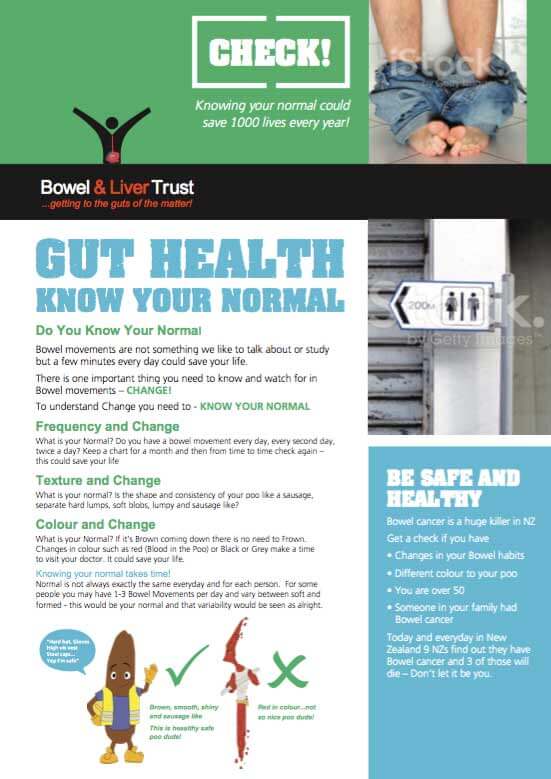
The treatments for bowel cancer include chemotherapy, immunotherapy, surgery and radiation treatment. The type of treatment depends on the size of the cancer, its location and whether it has spread. You may hear these talked about as the stage of the cancer and the grade of the cancer. Read more about staging and grading.(external link)
Your general health and your wishes are also important in the decision making. In some cases you may want to seek a second opinion. Read more about getting a second opinion.(external link)
Chemotherapy and immunotherapy are often recommended as part of a treatment plan. They may have side effects but, if they’re recommended, it generally means the benefits are likely to outweigh the adverse effects. Read more about chemotherapy and targeted therapies for bowel cancer(external link).
Note: Some medicines for treating bowel cancer are fully funded in Aotearoa New Zealand but others are not. You may be offered participation in a clinical trial. Read more about unfunded medicines and clinical trials.(external link)
If bowel cancer is detected early, there’s a good chance it can be treated successfully. However, a complete cure is not always possible and the cancer may return.
If the cancer is advanced and has spread to other part of your body (also called secondary or metastatic cancer), you will be offered different treatment options. Read more about advanced bowel cancer(external link).
The links above lead to more detailed information provided by Bowel Cancer NZ.