The intra-uterine device, or IUD, is a form of contraception that prevents pregnancy.
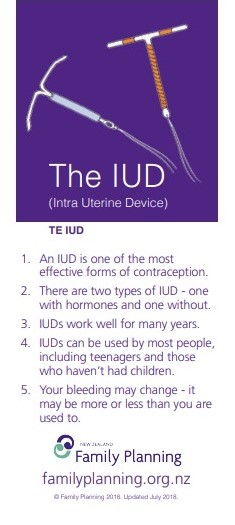
- An IUD is a small, T-shaped plastic device that is inserted into your uterus (womb) and has a plastic string tied to the end which hangs down through the cervix into the vagina.
- It is a long-acting form of contraception, which means that once it is inserted you don't have to remember about it every day or every time you have sex.
- Its effect is reversible which means that your natural fertility returns after the IUD is removed.
| Type of medicine | Also called |
|---|---|
|
|