On this page you will find videos on:
- Drawing up insulin
- How to use an insulin pen
- Giving the first injection
- Giving an insulin injection to a toddler
- Using a log book to record blood glucose levels
- Supporting your child with diabetes
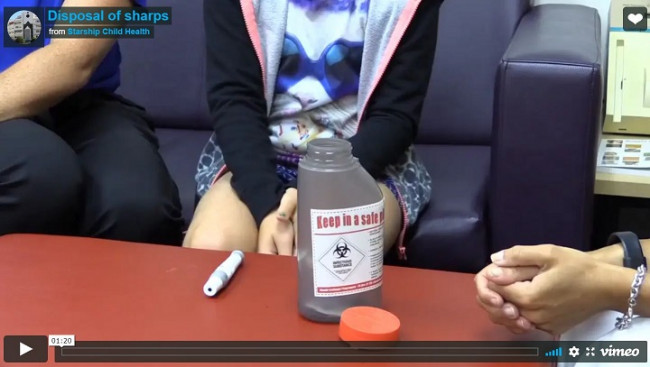
- Disposal of needles
1. Drawing up insulin
 (external link)
(external link)
(Starship Children's Health, NZ)
2. How to use an insulin pen
 (external link)
(external link)
(Starship Children's Health, NZ)
3. Giving the first injection
 (external link)
(external link)
(Starship Children's Health, NZ)
4. Giving an insulin injection to a toddler
 (external link)
(external link)
(Starship Children's Health, NZ)
5. Using a log book to record blood glucose levels
 (external link)
(external link)
(Starship Children's Health, NZ)
6. Supporting your child with diabetes
 (external link)
(external link)
(Starship Children's Health, NZ)
7. Disposal of needles
 (external link)
(external link)
(Starship Children's Health, NZ)