If you miss 1 pill
If you forget to take a pill, take it as soon as you remember, and take the next one at the normal time (even if this means taking 2 pills together). If you miss 1 pill, you are still protected from pregnancy.
If you miss 2 or more pills
Take a pill as soon as you remember and the next one at the normal time (even if this means taking 2 pills together). Depending on how you are taking the pill, you might need to take other steps to protect yourself from pregnancy. Check out the information below for your pill-taking options.
| It can be complicated working out what to do if you have missed some pills, so if you are not sure what to do ask your doctor, nurse or pharmacist as soon as you can. The following is some guidance. |
Options 1 or 2: Traditional or other tailored (not continuous) regimens
During week 1 (ie, after starting the pill for the first time or in the week after the non-hormone pills)
If 2 or more active hormone pills are missed, you need to go back to taking hormone pills daily AND use condoms or avoid having sex for the next 7 days. If you have had unprotected sex in the week before or during this first week, contact your doctor, nurse, pharmacist or Healthline 0800 611 116 for advice. You may need to use emergency contraception.
During week 2 or any weeks of a tailored regimen that are not within the first or last weeks of active hormone pill taking
If 8 or more hormone pills are missed, you need to go back to taking hormone pills daily AND use condoms or avoid having sex for the next 7 days.
During week 3 or in the week prior to a scheduled break from hormone pills
If 2 or more of the last 7 hormone pills are missed, you should skip the non-hormone pills and go straight on to taking the hormone pills from the next packet. If you decide to continue with the non-hormone pills, you will need to use condoms or avoid having sex until you have taken 7 hormone pills in a row.
Option 3: Continuous regimen
If you have been taking the hormone pills correctly for at least 7 days in a row before the missed pills, up to 8 pills can be missed and you are still protected from pregnancy.
If you have missed more than 8 pills in a row, OR have not been taking the hormone pills for at least 7 days in a row before the missed pills, then your pill will not be working. You need to start taking hormone pills AND use condoms or avoid having sex for the next 7 days. If you have had unprotected sex during or after missing more than 8 pills in a row, contact your doctor, nurse, pharmacist or Healthline 0800 611 116 for advice. You may need to use emergency contraception.



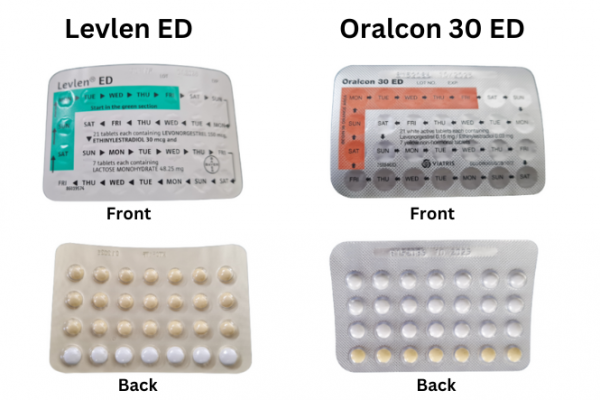
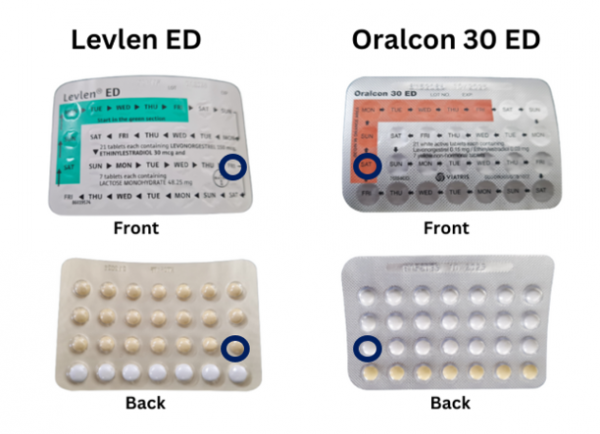
 Some packs of the combined pill have 21 active pills and 7 non-active sugar pills. The non-active sugar pills are also called non-hormonal placebo or reminder pills. These pills are meant to help you remember to take your pill every day and start your next pack on time.
Some packs of the combined pill have 21 active pills and 7 non-active sugar pills. The non-active sugar pills are also called non-hormonal placebo or reminder pills. These pills are meant to help you remember to take your pill every day and start your next pack on time.