- The link between food and mood is clear: what you eat affects your mental wellbeing. In fact, poor diet may not only be a reaction to feeling depressed, but may be one of the factors that trigger it.
- If you are feeling depressed or anxious, you are more likely to want to eat more unhealthy foods (such as potato chips and takeaways) and eat fewer healthy foods (such as fresh fruit and vegetables). But, eating unhealthy foods can actually make you feel worse.
- You can improve your mental wellbeing by making changes to your diet. And luckily, the same eating habits that keep you mentally well are those that support your physical health too.
- Choose a diet high in vegetables, fruits, unprocessed grains and fish, with smaller portions of lean meat and dairy – and limit those sugary, salty and processed foods.
Low or no data? Visit zero.govt.nz, scroll down the page then click on our logo to return to our site and browse for free.
Food and mood
Key points about food and mood
- What you eat affects not only your physical health but also your mental health.
- Eating some foods can improve your mood and mental wellbeing, while other foods can have a negative impact on how you feel.
- If you are feeling depressed or anxious you may be tempted to eat unhealthy foods (eg, potato chips) fewer healthy foods (eg, fresh fruit and vegetables) but that can actually make you feel worse.
- Positive changes in your diet can improve your mental wellbeing.

Just as sleep and exercise are key to feeling good, food also affects your mood. Like the rest of your body, your brain needs fuel to function. And just like filling up your car, putting in the right kind of fuel is key to how well your brain performs – including how well you are mentally and emotionally.
A recent study showed that the more people improved their food choices, the more their depression improved. Food is linked to the hippocampus, a key area of your brain involved in learning, memory and mental health. People with healthy diets have more hippocampal volume than those with unhealthy diets.
As well as your brain, your gut is the other part of your body that plays a key role in your mood. Everything you eat passes through your intestine (gut). Your gut is home to billions of bacteria and other mircroorganisms (bugs), known as your gut microbiome. These bugs are involved in many functions critical to your health and wellbeing. Therefore, eating foods that support your gut microbiome will support your mental health. Read more about gut health and mental health in the section below.
Although we don’t yet know exactly which bugs are needed for the optimal mix of gut bacteria, we do know that greater diversity of bugs is associated with better health outcomes(external link). And what promotes a greater variety of gut bugs? The simple answer: fibre-rich whole-foods(external link).
Video: How to manage your mood with food | 8 tips
This video may take a few moments to load.
(Mind, the mental health charity, UK, 2018)
Food choices that meet the Eating and activity guidelines for NZ Adults(external link), as well as Mediterranean eating patterns, can reduce the risk of getting depression. What does that look like in terms of food? To quote food author Michael Pollan: “eat food, not too much, mostly plants”.
Eat food, mostly plants
“Eat food” means to eat real food – vegetables, fruits, nuts and seeds, whole grains, fish and meat – and avoid highly processed foods. People who eat a diet high in whole foods are up to 35% less likely to develop depression than people who eat less of these foods. A University of Otago study found that young adults who ate more fruit and vegetables for just 2 weeks increased their feelings of vitality and wellbeing.
Rather than only eating cooked fruit and vegetables, each day have some of them raw.
An eating pattern that includes a wide range of foods includes the following:
- vegetables (eg, carrots, dark leafy greens, cucumber)
- fruits (eg, bananas, apples, citrus, berries)
- legumes (eg, lentils, chickpeas, beans)
- wholegrains (eg, rice, oats, breads)
- nuts and seeds
- oily fish and lean meats
- good oils (eg, most plant-based oils).
If you eat a wide range of foods the nutrients should take care of themselves, including the main nutrients associated with depression:
- Omega 3 fatty acids – because of its anti-inflammatory properties and effects on transmitting the hormones dopamine and serotonin, omega 3 has a role in brain development and functioning. If you don’t have enough omega-3, it can contribute to mental health problems.12 These are found in oily fish (salmon, tuna, sardines and anchovies, plant-based oils, walnuts, flax and chia seeds and dark green leafy veggies, as well as some fish oil supplements.
- B group vitamins – these help regulate neurotransmitters and immune function. They can be found in green leafy veggies, legumes and whole grains. B12 is in fish, beef, lamb, poultry, eggs and milk and some fortified breakfast cereals.
- Vitamin D – for optimal brain function, mood and critical thinking – and present in fatty fish, eggs, dairy foods and sunlight!
Not too much
- Cut down on sugar, salt and highly processed foods (eg, takeaway meals, packaged snack foods and processed or smoked meats).
- Limit caffeine (which may cause or exacerbate anxiety).
- If you drink alcohol, reduce your long-term health risks by drinking no more than:
- 2 standard drinks a day for women and no more than 10 standard drinks a week
- 3 standard drinks a day for men and no more than 15 standard drinks a week.
- This should include at least 2 alcohol-free days every week.
- Read more about alcohol and low-risk drinking.
Your gut microbiome also activates a neural pathway that travels directly between your gut and your brain, called the gut-brain axis. Because of this pathway, the food you digest in your gut affects the messages sent to your brain. This means that what is happening in your digestive system affects your emotional and mental wellbeing.
How does gut health affect mental health?
Everything you eat passes through your intestine (gut). Your gut is home to billions of bacteria and other micro-organisms (bugs), known as your gut microbiome. These bugs are involved in many functions critical to your health and wellbeing. A healthy gut microbiome:
- provides a strong barrier against toxins and “bad” bacteria
- aids absorbtion of nutrients from your food (digestion)
- supports the functioning of neurons (nerve cells) that line your gut wall
- helps reduce inflammation.
Your gut microbiome also activates a neural pathway that travels directly between your gut and your brain, called the gut–brain axis. Because of this pathway, the food you digest in your gut affects the messages sent to your brain. This means that what is happening in your digestive system affects your emotional and mental wellbeing. Therefore, eating foods that support your gut microbiome will support your mental health.
What foods support a healthy gut microbiome?
Although it's not yet known exactly which bugs are needed for the ideal mix of gut bacteria, it is known that greater diversity of bugs is associated with better health outcomes. And what promotes a greater variety of gut bugs? The simple answer is fibre-rich whole-foods.
- Fibre-rich whole foods help support a healthy gut. These include plant foods such as vegetables, fruit, whole-grains, legumes, nuts and seeds.
- You can also promote a healthy gut by eating bacteria itself in the form of fermented food such as kimchi, kefir and sauerkraut.
- The benefits of eating fibre-rich food or fermented food only last for as long as you are eating them (or shortly thereafter).
- This means that if you want to get their health-benefiting rewards, you need eat them every day and ideally with every meal.
- Simple ways to increase dietary fibre intake include swapping white bread or white rice for wholegrain bread or brown rice, or snacking on fruit or adding a cup of mixed vegetables with lunch or dinner.
A day-to-day diet lacking in fibre starves the gut microbiome and can lead to them eating the mucus that lines and protects your gut wall. Evidence suggests that if your gut microbiome consume too much of your gut wall, damaging inflammatory processes may kick in.
The following links provide further information about food and mood. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Diet and nutrition infographic(external link) Food and Mood Centre, Australia
Feeding minds – the impact of food on mental health(external link) Mental Health Foundation, UK
Diet and mental health(external link) Food and Mood Centre, Australia
Gut microbiota and diet – an introduction(external link) Food and Mood Centre, Australia
Food and mood – Improving mental health through diet and nutrition(external link) Future Learn
Food and Nutrition: The Truth Behind Food Headlines(external link) Online Course Future Learn. Paid course. 2 hours a week for 3 weeks. This course is designed for anyone who is losing trust in media headlines about how what we eat affects our health and who wants to get to the truth.
Resources
Healthy eating and depression(external link) Mental Health Foundation, UK
Food and mental health(external link) Mind UK
Food for your mood [PDF, 593 KB] Western Bay of Plenty PHO, NZ
Online courses
Food for Thought: The Relationship Between Food, Gut and Brain(external link) Future Learn (paid course) 4 hours a week for 5 weeks
This course is open to everyone, but may be of particular interest to psychologists or people working in health and well-being. No previous experience is required, though a background knowledge of biology or psychology may help.
References
- Lassale C, Batty GD, Baghdadli A, et al. Healthy dietary indices and risk of depressive outcomes – a systematic review and meta-analysis of observational studies(external link)
- Nutritional psychiatry – your brain on food(external link) Harvard Health, US, 2015
- Evrensel A, Ceylan ME. The gut-brain axis – the missing link in depression(external link) Clin Psychopharmacol Neurosci. 2015 Dec;13(3):239–244.
- Hannah D. Holscher(2017) Dietary fiber and prebiotics and the gastrointestinal microbiota, Gut Microbes(external link), 8:2, 172-184.
- Diet and the gut microbiota(external link) Food and Mood Centre, Australia
See our page Food & mood for healthcare providers
Brochures
Mental Health Foundation UK
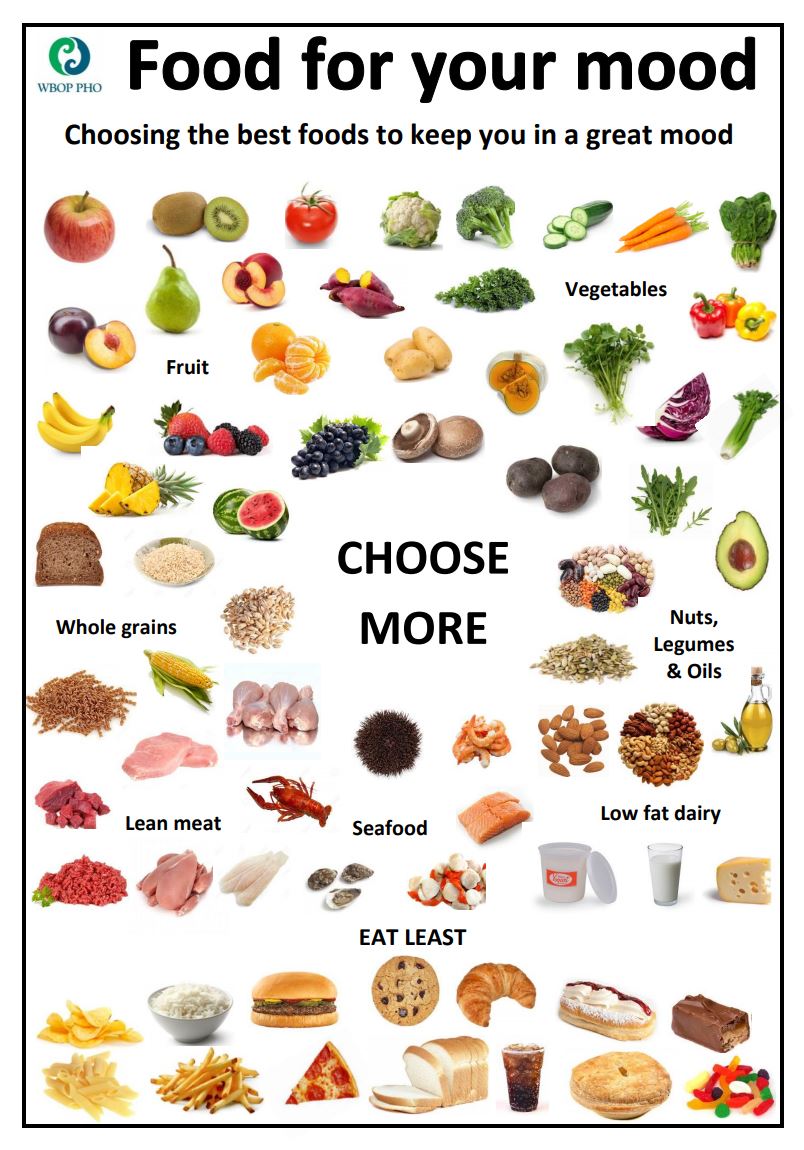
Western Bay of Plenty PHO, NZ
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Julie Carter, registered dietitian, Auckland DHB
Last reviewed:
Page last updated:





