Here is a way you can have your baby next to your bed but not actually in your bed with you.
 Image credit: Canva
Image credit: Canva
If you want to share a bed or sleeping space with your baby, you must have a separate bed for your baby that can be placed in your bed.
There is a range of baby beds you can choose that allow your baby to share your bed while sleeping in their own space, such as a wahakura or pepi pod(external link). Wahakura are hand-woven sleep spaces for pēpē made out of harakeke (flax) and using the tradition of rāranga (Māori weaving practices).
Tips on how to co-sleep with your pēpi
Use a wahakura
A wahakura is a small, flax-woven bed that can be fitted with a mattress that allows parents to have their baby in their bed but contained in a safe space. This helps protect against accidental suffocation caused by a parent or caregiver rolling onto their baby, or the baby being smothered by blankets. Wahakura were piloted in Gisborne in 2006 and Hawke’s Bay in 2007 and later rolled out around other parts of the country.
Use a pepi-pod
Pepi-pods are made from polypropylene plastic that can be fitted with a mattress and bedding. Like the wahakura, they are placed on the parent’s bed but provide a buffer of protection against accidental suffocation.
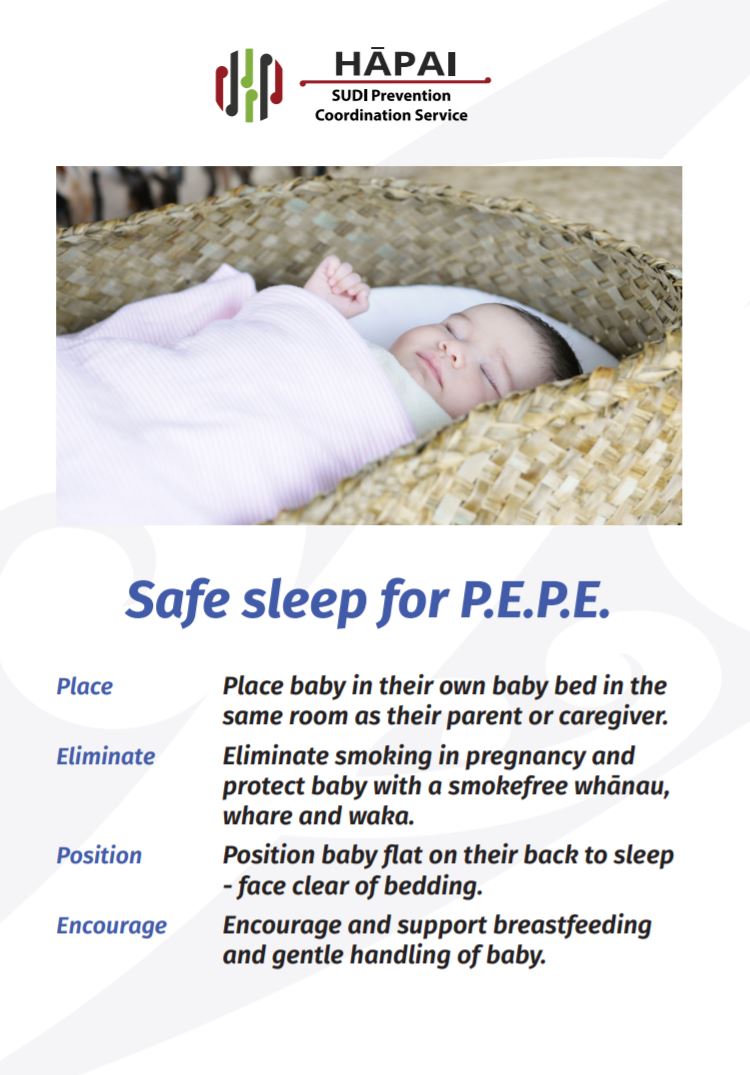
Put them to sleep on their back
Put your baby to sleep on their back with their feet right at the foot of their sleeping place. This helps to keep their airways clear and stop them burrowing under the blankets. Always put your baby back to sleep in their sleeping place (eg, wahakura or pepi-pod) after feeding so you don’t fall asleep on them.
Provide a smoke-free environment
Having a smoke-free home and car keeps your baby free from second-hand cigarette smoke, which is very harmful to them. Also, ensure the person looking after your baby is free from drugs and alcohol so they can be alert to your baby’s needs.
Breastfeed your baby
If possible, breastfeed only for the first 6 months. It’s advisable to keep breastfeeding until your baby is a year old if you can because breastfeeding helps protect your baby against SUDI.
Uncover their head and face
Make sure your baby’s head and face are free from things that may suffocate them like a pillow, bumper pad or hat. Don’t put any stuffed toys or playthings in your baby’s sleeping place that they could suffocate or choke on, including teething necklaces.
Dress them for the temperature
Your baby needs to be kept at a comfortable temperature so they don’t overheat. Make sure your baby doesn’t have too many clothes or blankets on. Having your baby in one more layer of clothing than you would wear is a good guide.
Use a firm and well-fitting mattress
Having a firm, flat mattress helps keep your baby’s airways open and stops them rolling. Make sure there are no gaps between your baby’s mattress and the side of the wahakura or pepi-pod.




 Image credit: Canva
Image credit: Canva