There are many different STIs. The following is a brief description of the most common ones. Click on the links below for more detailed information.
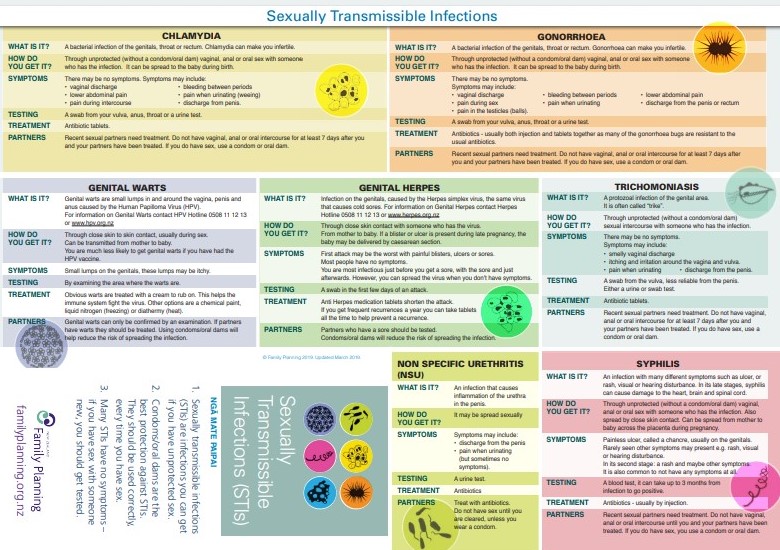
Chlamydia
Chlamydia is the most commonly diagnosed STI in New Zealand. It affects both men and women. Most people who have chlamydia don't show any symptoms – but they can still infect other people. Chlamydia can be easily treated with antibiotics. Left untreated, chlamydia can cause infertility.
Read more about chlamydia.
Gonorrhoea
Gonorrhoea is very common in people aged under 25 years. About half of women and one in 10 of men who have gonorrhoea don't experience any symptoms and don't know they're infected. In women, gonorrhoea can cause pain or a burning sensation when urinating (peeing), a vaginal discharge (often watery, yellow or green), pain in your lower abdomen (tummy) during or after sex, and bleeding during or after sex or between periods, sometimes causing heavy periods.
In men, gonorrhoea can cause pain or a burning sensation when urinating (peeing), a white, yellow or green discharge from the tip of your penis, and pain or tenderness in your testicles. It's also possible to have a gonorrhoea infection in your rectum, throat or eyes.
Read more about gonorrhoea.
Syphilis
Syphilis enters your body through tiny breaks in your skin, mainly in your genital area or mouth. Many people do not get any symptoms and would not know they had syphilis without having a blood test. Treatment is normally with injections of an antibiotic called benzathine penicillin. If left untreated, the syphilis bacteria eventually causes damage to your internal organs. People without symptoms can still develop these problems later if their syphilis is not treated.
Read more about syphilis.
Trichomoniasis
Both men and women can get trichomoniasis, but it is more common in women. In women, the infection can cause a frothy yellow or watery vaginal discharge that has an unpleasant smell, soreness or itching around your vagina, and pain when passing urine (peeing).
In men, trichomoniasis rarely causes symptoms. You may experience pain or burning after passing urine (peeing), a whitish discharge, or an inflamed foreskin.
Read more about trichomoniasis.
Human papillomavirus (HPV) and genital warts
Genital warts are caused by the human papilloma virus (HPV). They appear as small fleshy growths, bumps or skin changes, on or around your genital or anal area. The warts are usually painless, but you may notice some itching or redness. Sometimes, they can cause bleeding. You don't need to have penetrative sex to pass the infection on because HPV is spread by skin-to-skin contact. Several treatments are available for genital warts, including creams and freezing the warts (cryotherapy).
There is now a vaccine available that protects against HPV including the types that cause genital warts. It is recommended to be given at age 11–12 years but is free in New Zealand for anyone aged 9–26 years.
Read more about human papilloma virus (HPV), HPV vaccine and genital warts.
Genital herpes
Genital herpes is caused by a virus known as the herpes simplex virus (HSV).The symptoms of genital herpes are similar to cold sores found on your mouth, except they appear on your genital skin. Small, painful blisters or sores usually develop, which may cause itching or tingling, or make it painful to urinate (pee). After you've been infected, the virus can remain dormant (inactive) and certain triggers can reactivate the virus, causing the blisters to develop. Most people with genital herpes don’t have any symptoms and the virus can be passed on by people with no symptoms. Genital herpes cannot be cured; however, symptoms can be treated.
Read more about genital herpes.
Hepatitis B
Hepatitis B is a viral infection that causes inflammation of your liver. Some people do not have any symptoms, but others can have symptoms such as feeling sick or vomiting, lack of appetite, flu-like symptoms (such as tiredness, general aches and pains or headaches), abdominal (tummy) pain, clay-coloured bowel motions and/or dark-coloured urine and yellowing of your skin and eyes (known as jaundice). One of the most effective ways to avoid getting hepatitis B is get immunised with the hepatitis B vaccine.
Read more about hepatitis B.
Human immunodeficiency virus (HIV)
HIV is caused by the human immunodeficiency virus which causes damage to your body's immune system and impairs your ability to fight disease-causing organisms. HIV is most commonly passed on through unprotected sex. Without treatment, some people with HIV may develop the potentially life-threatening condition known as acquired immunodeficiency syndrome (AIDS). There's no cure for HIV, but there are treatments that allow most people to live a long and otherwise healthy life.
Read more about HIV.
Pubic lice
Pubic lice, also called crabs, are usually found in pubic hair but can live in your underarm hair, body hair, beards and sometimes eyebrows or eyelashes. They are easily passed to others through close genital contact. The lice crawl from hair to hair but don't jump or fly from person to person. It may take several weeks for you to notice any symptoms. Most people experience itching, and you may notice the lice or eggs on your hairs. Pubic lice are treated with special creams, lotions or shampoos available from your pharmacy or your GP. You don't need to shave off your pubic hair or body hair.
Read more about pubic lice.