While there's no cure for PCOS, there are many effective ways to reduce the symptoms and long-term effects on your health. The key to managing PCOS well is working in partnership with your healthcare team to find the best strategies for you. You may want to include your whānau and friends in your care.
Your symptom experience and quality of life, together with your concerns, values, and priorities are really important in any conversations you have about how to manage your PCOS.
PCOS support groups can also be great sources of emotional and peer-support.
There are apps specifically designed to help people with PCOS to understand and manage their condition better. Read more about the AskPCOS app.
Managing PCOS with lifestyle
A healthy lifestyle is recommended for all people with PCOS because it has benefits for all the features of the condition.
A healthy lifestyle includes:
- Eating a balanced and nutritious diet: No one diet is better than another for PCOS. Working with a healthcare provider is important for choosing an approach that is flexible, sustainable, allows for your food preferences, and avoids diets that are too restrictive or aren't nutritionally balanced. Read more about healthy eating.
- Being as active as possible: No one type of exercise is better than another if you have PCOS. Try to include exercise in your daily routine, talk to your healthcare provider about how to be active in a way that suits you and your lifestyle. Read more about ways to increase your activity.
- Maintaining a healthy weight: Weight management is linked to significant improvements in PCOS. You may gain weight and find it difficult to lose. You may wish to work with a healthcare provider to develop tailored goals and plans. Read more on managing your weight at the end of this section.
- Avoiding smoking and excessive drinking: Read more about how to quit smoking and alcohol and harmful drinking.
Managing PCOS with medicines
Lifestyle management is recommended for everyone with PCOS. There are also a number of medicines used to manage the different symptoms of PCOS, including medicines for acne, excess hair growth, problems with your periods and fertility issues. Some medicines may help with more than 1 symptom. PCOS affects everyone differently and your healthcare provider should work with you to decide which medicines best meet your needs. All medicines have different benefits, risks and side-effects to consider.
Contraceptive pill
The combined oral contraceptive pill is commonly prescribed to help you keep your periods regular and reduce excess hair growth by reducing the activity of the hormone testosterone. Your healthcare provider will discuss which combined oral contraceptive pill will best suit you. Generally, you will be started on a lower dose preparation or one with fewer side effects. Higher doses are used for severe symptoms.
Progestogen
You may be prescribed progestogen (a synthetic version of the hormone progesterone) so you have regular periods. Examples of progestogen are Medroxyprogesterone (Provera) and norethisterone (also called Primolut N).
Metformin
Metformin is commonly used for type 2 diabetes, but it can also help to reduce some symptoms of PCOS. It helps your body make better use of the insulin it produces. It can help with weight loss, blood pressure and may help with irregular periods.
Metformin should be used together with increased exercise and a nutritious diet, not as a replacement for a healthy approach to lifestyle. Read more abut metformin for PCOS.
Anti-androgen medicines
Anti-androgen medicines have a limited role in managing PCOS but may be considered if other therapies haven't been effective or can’t be used.
Spironolactone is used to reduce male-pattern hair growth and acne. It can reduce androgen levels, but it can take up to 6 months of daily use to work well. Read more about spironolactone.
Isotretinoin is used for severe acne that hasn’t been helped by other treatments. It shouldn't be used in pregnancy as there is a high risk of permanent damage to the unborn baby. Read more about isotretinoin and acne treatments.
Managing fertility
Having PCOS doesn't mean you can't get pregnant. Pregnancy can often be successfully achieved naturally or with assistance. If you have PCOS, the hormonal imbalance sometimes interferes with the growth and release of eggs from your ovaries (ovulation). If you don't ovulate, you can't get pregnant. Your healthcare provider or a fertility specialist can talk with you about ways to help you ovulate and increase your chance of getting pregnant.
A reproductive life plan and preconception care is recommended for people with PCOS, including healthy lifestyle, prevention of excess weight gain, and optimising preconception risk factors. It's important to have your blood pressure measured if you're planning a pregnancy or seeking fertility treatment. Excess weight is important because it can affect the chances of pregnancy, miscarriage and live birth rates following fertility treatment.
PCOS and pregnancy
In pregnancy PCOS increases the risk of:
It's important that your healthcare provider or midwife knows you have PCOS so they can do regular checks and give you the best support during your pregnancy.
Managing excess hair
Mechanical laser and light therapies are effective for removing excess face and body hair. These options should be considered for reducing hirsutism and its impact on your quality of life, depression and anxiety.
Managing your weight
Managing your weight is associated with significant improvements in PCOS. Lifelong healthy lifestyle strategies and prevention of excess weight gain are very important in PCOS for reproductive, metabolic, and psychological health. You may wish to work with a healthcare provider to develop tailored (personalised) goals and plans.
Having PCOS may mean you're more likely to gain weight and have greater challenges with weight management. Weight stigma is a combination of negative attitudes, stereotypes, and prejudice about high body weight. Weight stigma is common and can be harmful to people with PCOS and unhelpful to PCOS management.
Having a healthy lifestyle has benefits for people with PCOS even without weight loss. While higher weight is a risk factor for PCOS and its complications, it’s only 1 indicator of health.
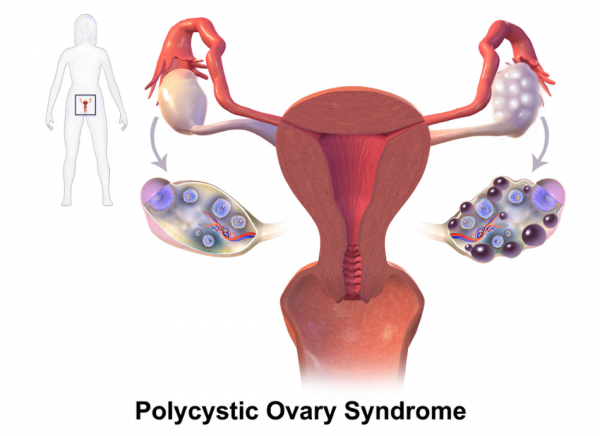 Image credit: BruceBlaus via Wikimedia Commons(external link)
Image credit: BruceBlaus via Wikimedia Commons(external link)








