Your pancreas is a small organ located behind your stomach and below your ribcage. It's a part of your digestive system. It releases enzymes, or digestive juices, into your small intestine to further break down food after it has left your stomach. It also secretes the hormone insulin into your bloodstream to regulate your glucose levels.
The image below shoes the location of your pancreas.
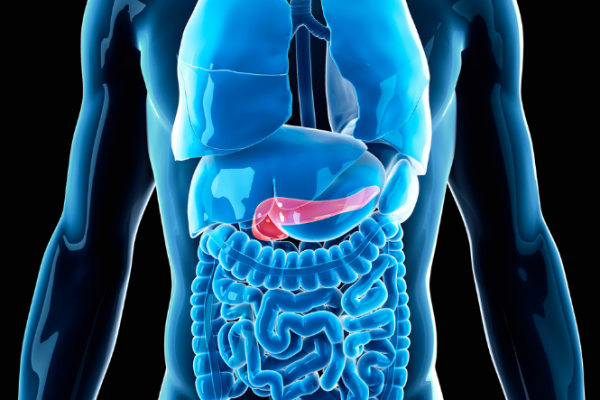
Image credit: Canva
Chronic pancreatitis happens when your pancreas becomes permanently damaged from inflammation. This inflammation is usually caused by heavy drinking, although smoking has also been found to be linked to chronic pancreatitis. The inflammation causes scarring and damage to parts of the pancreas, which affect its ability to produce digestive enzymes and insulin.
Chronic pancreatitis can affect people of any age, but is most common in men between 45 and 54 years of age.
Having chronic pancreatitis increases your risks of getting pancreatic cancer. Treatment manages symptoms but it can't repair damage. This means chronic pancreatitis can affect your life quite a lot, and getting support is important.
Video: Chronic pancreatitis signs and symptoms
This video may take a few moments to load.
(The National Pancreas Foundation, US, 2013)






