Put simply, too much weight or being underweight is the result of an energy imbalance. This means too much (or too little) energy (kilojoules/calories) in the form of food is put into your body and not enough (or too much) energy is used up through exercise and daily movement.
But the reason for your body size is not as simple as energy in, energy out. There are many factors that influence body size such as medical conditions, medicines, genetics, age, ethnicity, food security and even where you live.
Social factors that are out of your control also affect what and how much you and your child eat. Many of us live in an environment where we are surrounded by less nutritious food choices. Healthy food can seem costly and can take time to buy and prepare, which can be difficult with our lifestyles. Picky eating is also a common challenge that parents may face when feeding their children.
Low or no data? Visit zero.govt.nz, scroll down the page then click on our logo to return to our site and browse for free.
Body size and health in children
Key points about supporting healthy growth in children
- What's a healthy weight for one child might be quite different for another.
- A healthy body is one that, whatever shape, size or weight, is in a state of wellbeing and has enough energy and strength to do the things the person loves.
- To help your child have a healthy body it's best to support your whole whānau to live a healthy lifestyle.
- This includes having daily physical activity, following healthy eating guidelines, getting enough sleep and limiting screen time.
- It's common to believe that dieting and losing weight will help a person be healthy, but dieting is never healthy for children.
Doctors and healthcare providers use age-and sex-specific growth charts to help work out if your child is growing as expected for their height and age, or whether there are any sudden changes. A big drop or increase in weight within a short space of time can indicate health problems that may need to be looked into. But this is only one part of the picture.
As a parent you have the right to ask that your doctor or healthcare provider does not take your child’s weight or discuss weight in front of your child.
You can find out if your child is in the healthy weight range for their height using this BMI calculator(external link). But it is important to avoid weighing your child frequently at home so that they don’t develop stress or worry about their body size.
A healthy body is important for everyone, but especially for children who need good energy for growing, learning and playing. The tips below can support your child to have a healthy body.
Between 0–2 years of age your child is rapidly growing. It is also a key window of opportunity for you to help your child learn healthy eating patterns for life.
- For the first 6 months of life, your baby should only be fed breast milk. If you are not able to breastfeed, infant formula is a suitable alternative. When your baby is ready (around 6 months of age) you can start feeding them solids as well. You can continue to breastfeed for up to 2 years or longer.
- Healthy habits begin early. Use vegetables with your child’s first foods to help them learn to like the taste and textures. This guide(external link) will help you introduce the colourful world of fruit and vegetables.
- Your child may pull a surprised or ‘yuck’ face when introduced a new food. This is normal as they are learning about tastes and textures. Repeated exposure to foods will help your child learn to enjoy them.
- When preparing foods for your baby or toddler, do not add extra salt, sugar, honey, sweeteners or soy sauce so that they don’t develop a preference for sugary or salty foods.
- From 6 months of age offer your child water. Cow’s milk can be offered from 12 months of age. Read more information about introducing milk(external link).
- Do not offer your child tea, fizzy drink (including ‘zero’ options), fruit juice and artificially sweetened beverages. These products cause tooth decay and do not provide nutrition to support your child’s health.
For more information for nutrition for infants and toddlers see eating for healthy babies and toddlers(external link).
Food and eating
If children are provided food from all 4 food groups and encouraged to eat in tune with their own appetite, their body will naturally grow according to their most healthy weight, size and shape.
- Offer your child a variety of foods from these 4 food groups every day: vegetables and fruit; breads and cereals; milk and milk products; lean meats, chicken, seafood, eggs, legumes (beans and pulses), nuts and seeds.
- Offer 3 main meals and 2 or 3 healthy snacks at regular times throughout the day.
- Do not encourage continuous eating or grazing. Children need routine to stay attuned to their hunger-fullness body signals, both during and in between meals and snacks.
- Children have smaller stomachs than adults, so need smaller portions of food(external link). It is also normal for your child to eat lots of food on one day and then very little the next.
- Trust that your child is listening to their body and eating the right amount of food for their growth and energy levels.
- If you pressure kids to eat food when they are not actually hungry (eg, telling them to finish their plate), you are telling them not to trust the feeling of fullness. This can lead to a lifetime of not listening to your body's hunger and fullness cues. Pressuring your child to eat also makes mealtimes stressful for whānau.
- Create a relaxed and positive mealtime. Family mealtimes are a great way for your child to learn to eat, to connect as a family and share kai. Avoid having screens at the table.
- Children are more likely to eat a new food if they get the chance to get to know it first without the pressure to eat it. Get children involved in food preparation, gardening and food shopping. Play games and read books about food too.
- Offer water and milk only. Limit milk(external link) to 350 ml (about 1 ½ cups per day). Milk fills up toddler’s tummies, leaving less room for other nutritious foods.
For more information see healthy eating for children.
Physical activity, screen time and sleep
Children love to run around and move their bodies. If children are encouraged to engage in active play, their body will naturally develop according to their most healthy weight, size and shape.
- Make physical activity fun by finding lots of different ways for kids to play – running, jumping, skipping, riding a bike, bouncing on a trampoline, swimming, playing tag or backyard cricket. See these great physical activity ideas and tools(external link).
- You can encourage your child to be proud of their body by talking about all the amazing things it can do.
- The temptation of screens can make it difficult to encourage your child to get outside to play. You can find great tips for managing your child’s screen time here(external link).
- Make sure your child gets the recommended amount of sleep(external link) for their age. Sleep is related to appetite so when your child does not get enough sleep it is normal for them to feel hungrier.
- It is normal for your teenager’s appetite to increase as they are growing, so it is important to have plenty of healthy foods on offer from the 4 food groups: vegetables and fruit; breads and cereals; milk and milk products; lean meats, chicken, seafood, eggs, legumes (beans and pulses), nuts and seeds.
- As teenagers gain independence, it can be tempting for them to eat more energy dense snack foods and fast foods high in fat, sugar and salt. Support your teenager to make healthy food and activity choices for themselves. See what is healthy eating?
- Eat meals together as a family and be a positive role model by making healthy food and activity choices yourself.
If you are worried that your child is not at their most healthy weight, GPs, healthcare providers and dietitians can help you. They will assess whether there are any underlying health problems, and they can guide you to support your child’s growth.
You can also ask your doctor if there are local Māori health providers, Whānau Ora providers, Pasifika health providers or other community-based organisations that can support you.
As a parent, you can help your child a lot in these ways:
- Involve the whole family in making lifestyle changes following the healthy lifestyle tips listed above. Eating healthy food and being active every day makes a big difference to everybody’s wellbeing. For healthy family recipes see He kai(external link).
- Make mealtimes a positive and relaxed environment (without distractions).
- Teach your children to cook! This is an important skill for supporting wellbeing for life.
- Making sure your child has regular sleep times and gets lots of opportunity for active play.
A final note, it can be tricky to know what to say when your child asks a difficult question or makes an unexpected comment about body size.
The following links provide further information about supporting healthy growth in children. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Tips for parents(external link) SKIP, NZ
Resources
Eating for healthy babies & toddlers(external link) HealthEd, NZ, 2021
Eating for healthy children aged 2–12 years(external link) HealthEd, NZ, 2023
Healthy eating for young people(external link) HealthEd, NZ, 2021
Be active every day(external link) HealthEd, NZ, 2019
Healthy Heart Visual Food Guide Poster(external link) Heart Foundation, NZ
My goals chart – healthy kids(external link) Healthy Kids and Health Promotion Agency, NZ, 2022
BeSmarter – be body wise(external link) WaiKids & Sports Waikato, NZ
Tinana ora mo nga tamariki – physical wellbeing for children(external link) WaiKids & Sports Waikato, NZ
Helping your family to get active [PDF, 1.7 MB] Sport Auckland, NZ
Food portions(external link) Heart Foundation, NZ
How much sugar do you drink?(external link) Health Promotion Agency, NZ, 2014
Healthy swaps(external link) Health Promotion Agency, NZ, 2017
Sit less, move more, sleep well – active play guidelines for under-fives(external link) Ministry of Health, NZ, 2017
Sleep tips for young children Ministry of Health, NZ, 2016
Introducing the colourful world of fruits and vegetables to babies and toddlers(external link) 5+ A Day, NZ, 2020
References
- Food and nutrition guidelines for healthy children and young people(external link) Ministry of Health, NZ, 2015
- How we eat(external link) Ministry of Health, NZ, 2017
- Your Child's Weight(external link) Nemours KidsHealth
- Body image – tips for parents(external link) BetterHealth, Australia
As a health professional, it is important to conduct conversations about body size with kindness and compassion. It is also important to remember that BMI is not the only indicator of health and that there are many factors that influence a person’s body size such as medical conditions, medication, genetics, ethnicity and social factors.
If a child’s weight/height is trending up or down across centiles over time, the underlying medical (or social) reasons for this should be explored by a GP or specialist.
It is common to believe that dieting and losing weight will help a person be healthy, but dieting is never healthy for children. Instead, we need to support whānau to make healthy lifestyle habits. The BeSmarter tool can be used to assist in your conversations with whānau.
BeSmarter – be body-wise(external link) Waikids, NZ
Healthy eating guidelines for New Zealand babies and toddlers (0–2 years old)(external link) Ministry of Health, NZ, 2021
Change talk(external link) (external link)– A 45-minute training tool for health professionals wanting to learn and/or practice motivational interviewing techniques
Food and nutrition guidelines for healthy children and young people(external link) Ministry of Health, NZ, 2015
Clinical guidelines for weight management in 2–5-year-olds(external link) Ministry of Health, NZ, 2016
Watch these series of videos(external link) from Te Hiringa Hauora. They are aimed at helping health professionals have conversations about childhood obesity. The videos cover a number of topics, including:
1. Starting the obesity conversation with families and whanau
2. Food in Pacific cultures
3. The role sleep plays in obesity
4. Building relationships with Māori and whanau
5. What is healthy eating?
6. Getting children moving more
Brochures
HealthEd, NZ, 2023
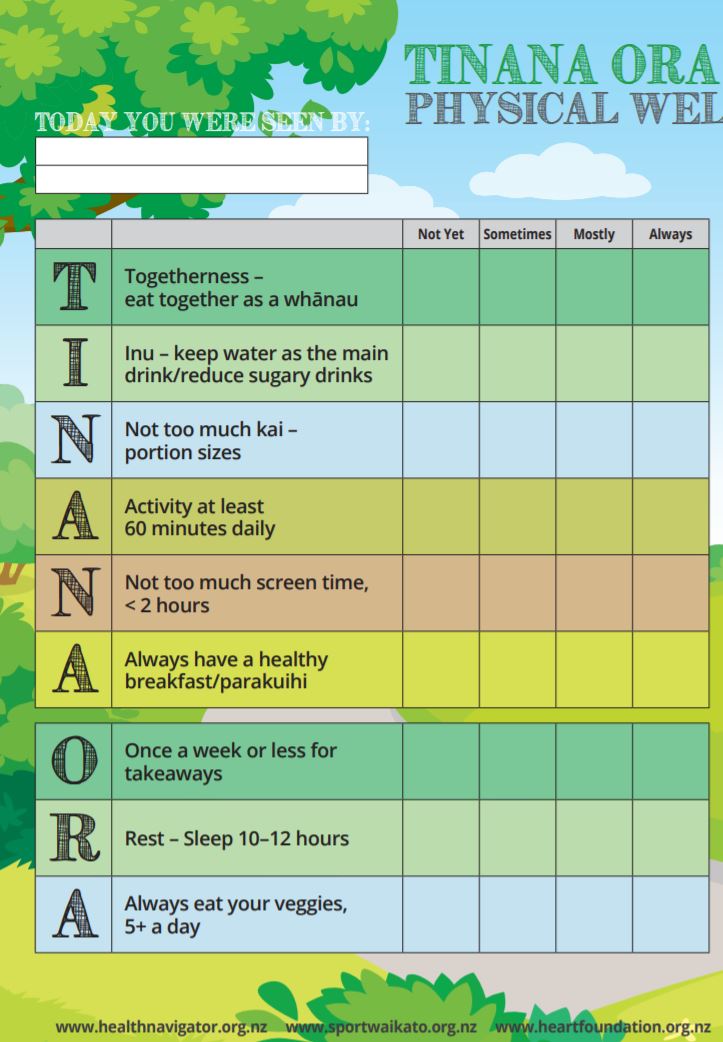
WaiKids & Sports Waikato, NZ
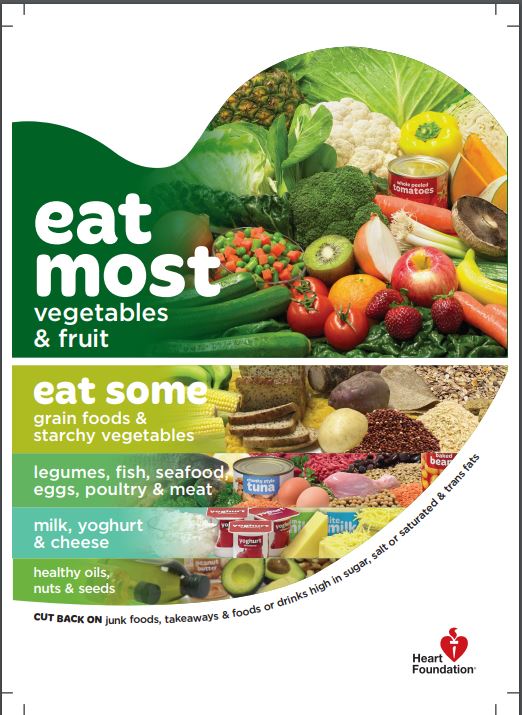
Heart Foundation, NZ
Credits: Gabrielle Orr, NZ Registered Dietitian, Auckland and Amanda Buhaets, NZ Registered Dietitian, Auckland
Reviewed by: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Last reviewed:
Page last updated:





