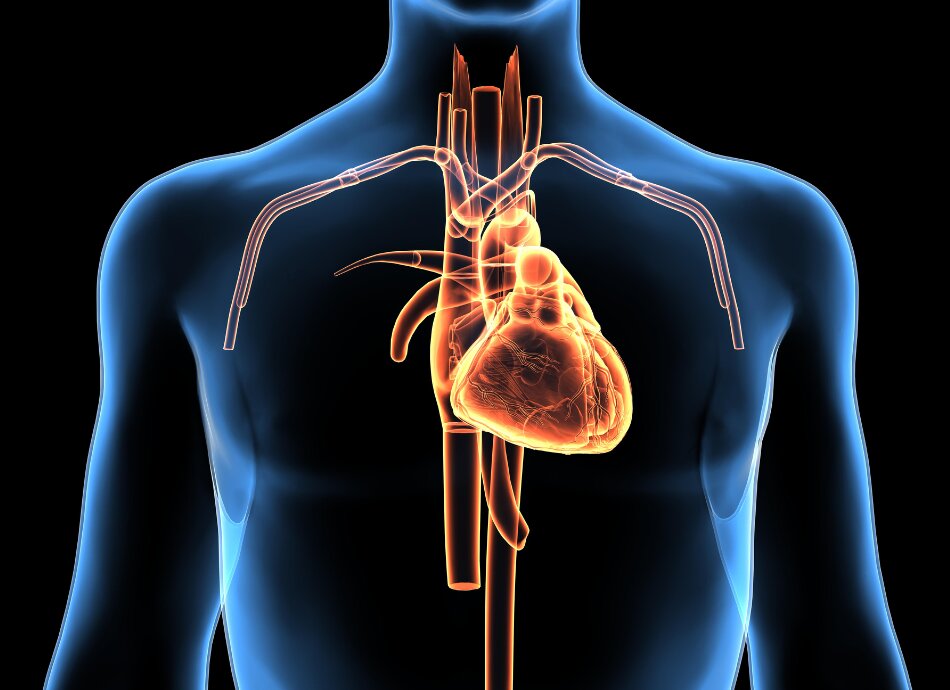
Myocarditis is inflammation (swelling) of your heart. It can affect the whole heart or just part of it. Myocarditis is a rare disorder. Each year about 100 people in Aotearoa New Zealand have myocarditis.
Video: Myocarditis: Causes, symptoms, diagnosis, treatment and prognosis | Kenhub
This video may take a few moments to load.