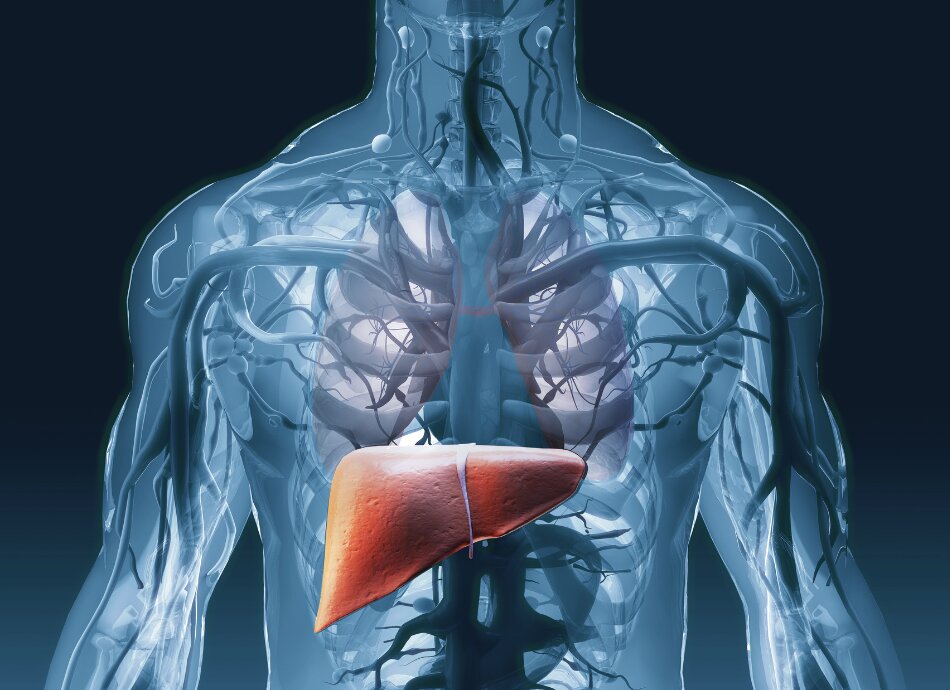
The main type of primary liver cancer that can affect adults is hepatocellular carcinoma (HCC).
- A less common type of liver cancer can start in the bile ducts that connect your liver to your bowel and gall bladder. This is known as cholangiocarcinoma or bile duct cancer.
- A very rare type of liver cancer that starts in your blood vessels is known as angiosarcoma.
- Hepatoblastoma is a form of liver cancer that affects only young children and is also very rare.
| The information on this page focuses on hepatocellular carcinoma (HCC) |
|---|