If your insomnia has become chronic, see your healthcare provider. Medical conditions or sleep-related disorders causing ongoing sleep problems may need to be investigated and managed. Your healthcare provider may also recommend cognitive behavioural therapy for insomnia (CBTi) or sleep (or bedtime) restriction therapy.
Cognitive behavioural therapy for insomnia (CBTi)
This is a form of cognitive behavioural therapy (CBT) designed especially for people with insomnia (CBTi). It involves a trained provider helping to identify the thoughts, feelings and behaviours that are contributing to your insomnia. It will be different for each person, as it depends on your own particular circumstances and needs, but can include:
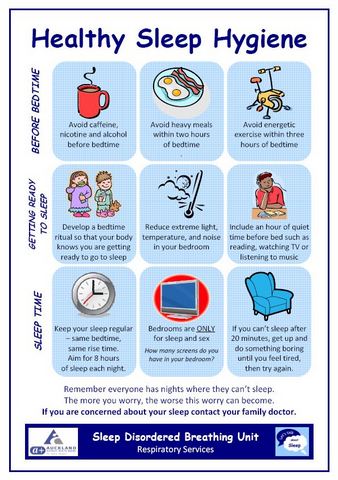
- education about sleep and sleep hygiene
- relaxation techniques
- sleep restriction (see below)
- addressing negative concerns and thoughts about sleep and insomnia
- homework (eg, keeping a sleep diary).
It’s been found to be very effective, with up to 80% of people experiencing improvement in their sleep.
It can be done by a trained doctor or sleep therapist. Just a Thought provides a free insomnia course you can do yourself online. Read more about how CBT-I works(external link) and the Just a Thought insomnia course(external link).
Online programmes include:
Sleep (or bedtime) restriction therapy
Sleep restriction therapy (also called bedtime restriction therapy) involves creating a new sleep schedule by limiting the amount of time you spend in bed, so that the time you spend in bed matches the time you actually sleep. Spending excessive time in bed may make insomnia worse because you can spend this time awake feeling worried or frustrated at being unable to sleep. Sleep restriction therapy aims to decrease the amount of time it takes to fall asleep, increase the amount of time spent sleeping before you wake in the night and enable you to have more regular sleep patterns.
Sleep restriction therapy is often a component of CBTi and is best done under the supervision of a healthcare provider.
- To undertake sleep restriction therapy, it’s important to keep a sleep journal and strictly stick to the sleep schedules that are part of the therapy.
- Sleep restriction therapy isn't suitable for everyone. For example, it’s not recommended for people in certain occupations (eg, transportation, construction and healthcare) as they might put themselves or others at risk if they attempt to work while sleep deprived.
- It also may not be suitable for people with some health conditions (eg, major illness or recent surgery, untreated sleep apnoea, seizure disorders that are not well controlled and untreated bipolar disorder).
- For sleep restriction therapy to work well, avoid falling asleep before bed (eg, while watching TV or reading) as this will decrease the need for sleep when you go to bed.
- You will probably feel sleepier than usual when you wake-up in the morning and during the day. You will start to need an alarm clock in the morning to ensure you don't sleep past the designated wake time. It's important to stick to the new schedule and not to nap during the day.
Sleep apps
There are a variety of sleep apps available for use on your smartphone or tablet that can be helpful if you have insomnia. Some apps track your sleep habits, similar to a sleep diary, to help you develop good sleep routines. Other apps help you to fall asleep by using calming visual graphics and relaxing music.