The word hernia means ‘something coming through’. The most common place for a hernia is the abdominal wall – a large sheet of muscle and tendon that helps hold all the abdominal content in place.
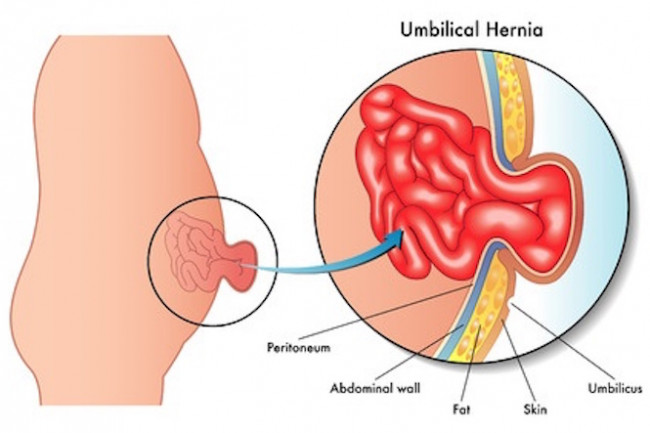
If there is an area of weakness in the wall, pressure from inside the wall can cause part of the abdominal contents (eg, the intestines) to be pushed through the opening. This resulting bulge is known as a hernia.
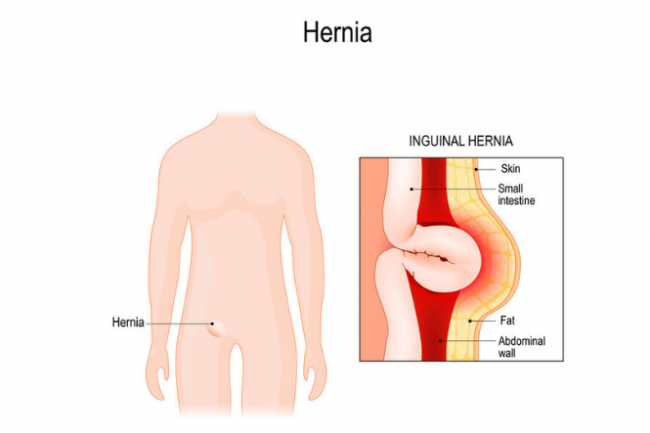
Image credit: 123rf
There are several common types of hernia:
- Inguinal hernias occur near your groin and are more common in men.
- Femoral hernias occur where your leg joins your body and are more common in women.
- Incisional hernias occur where you have a scar from surgery.
- Umbilical hernias occur near your naval (belly button) and are more common in newborns or people who are obese.
- Hiatus hernias occur when part of your stomach pushes up into the chest.
Hernias can affect anyone and many babies are born with hernias.