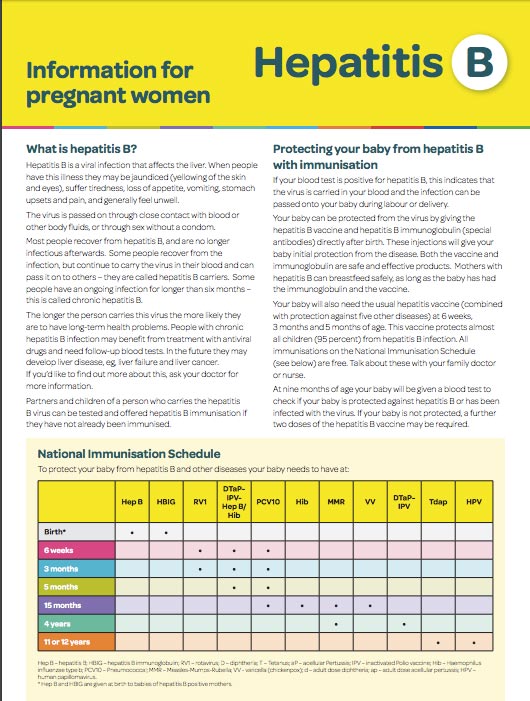
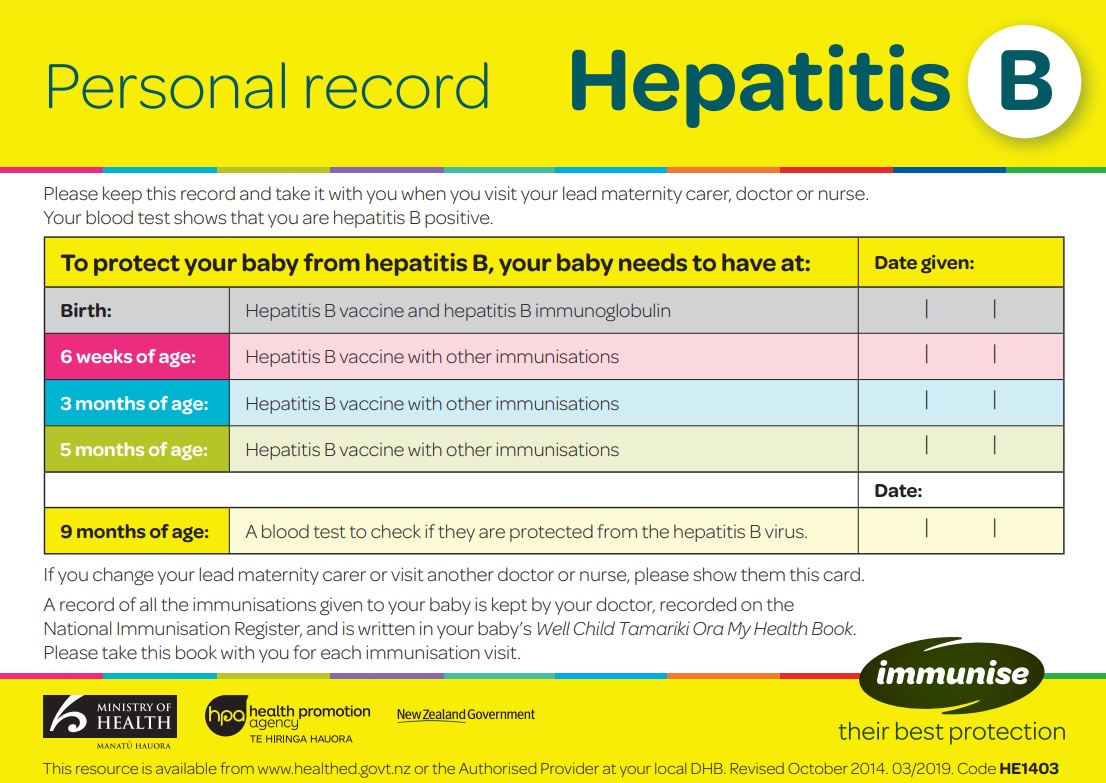
Hepatitis B (pokenga ate) is a virus that causes inflammation of your liver. If you have hepatitis B during pregnancy, you can pass the virus on to your baby. There are various medicines that can reduce the risk of transmission and protect your baby from hepatitis B.
- Most people who are carriers of the hepatitis B virus are unaware of this, because often there are no symptoms or only mild symptoms. Read more about hepatitis B and chronic hepatitis B.
- You can pass hepatitis B to your baby during the birth through contact with your blood and body fluids. This can happen with vaginal delivery or Caesarean section.
- During pregnancy, as part of your antenatal checks when you first see your lead maternity carer, you will be offered a blood test for hepatitis B.
- Hepatitis B doesn’t usually cause problems for you or your unborn baby during pregnancy. However, when babies and young children get infected (although they don’t tend to get sick) they're at much higher risk of remaining a hepatitis B carrier and developing ongoing liver problems later in life.
- There are various medicines that can reduce the risk of transmission (passing it on) and protect your baby from hepatitis B.

Image credit: Canva