Heartburn is when acid leaks from your stomach into your oesophagus (the tube that carries food from your mouth to your stomach). This can happen when the sphincter (which sits at the junction of your stomach and oesophagus like a valve) doesn't close properly. This could be due to high pressure in your stomach or when your stomach produces too much acid. Most people experience heartburn at some time in their life. The heart is not involved in heartburn.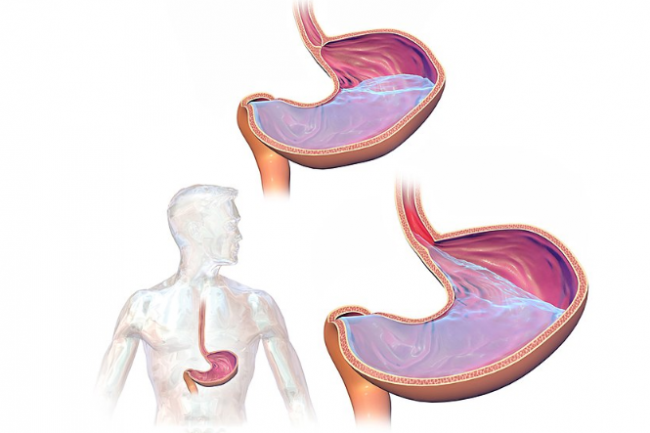
Image credit: commons.wikimedia.org
Indigestion (dyspepsia) is a group of symptoms that describe stomach pain or discomfort experienced after eating. Heartburn is one of these symptoms.







