Fluids: Give your child plenty of fluids to avoid dehydration. Encourage them to eat small, healthy meals or snacks.
Rest: Give them extra rest.
Clothing: Undress your child so they are just wearing a single layer (maybe a singlet and pants). Make sure the room is not too hot or too cold.
Check them regularly: You may need to give them extra cuddles and let them be closer to you.
Medicine: Give medication if needed and always follow the label to make sure it’s the right dose for your child’s age, weight and illness. See below for information on medication.
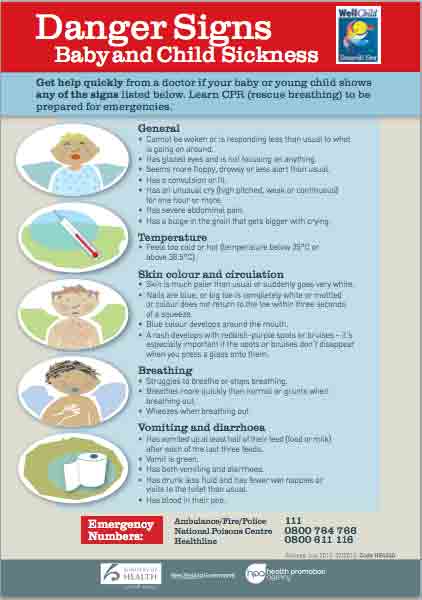
| Important: babies under 3 months old should be seen by a doctor |
|---|
|
It's OK to look after your child, or baby over 3 months old, at home as long as they are drinking and eating well and interacting with you.