Prediabetes occurs when the amount of glucose (sugar) in your blood is higher than normal but is not high enough to be diabetes. About 20% of the adult population is likely to have prediabetes.
Low or no data? Visit zero.govt.nz, scroll down the page then click on our logo to return to our site and browse for free.
Prediabetes | Tūraru mate huka
Also called impaired glucose tolerance
Key points about prediabetes
- Prediabetes (tūraru mate huka) is when your blood glucose is higher than normal, but not high enough to be diabetes.
- It increases your risk of getting type 2 diabetes and heart disease.
- Knowing you have prediabetes is a chance to make positive lifestyle changes.
- To manage or prevent it, keep to a healthy body weight, eat and drink wisely and stay active.

Yes, it is a concern because if you have prediabetes you have higher blood glucose levels than normal. This puts you at higher risk of developing type 2 diabetes and heart disease. However, following a healthy lifestyle is a very powerful way to prevent or delay type 2 diabetes developing.
Insulin is the hormone your body produces to control the glucose in your blood, keeping it in the healthy range. Prediabetes is an indicator that your body isn't using insulin as well as it should. In other words, your body is starting to become resistant to insulin. When your body resists insulin, the glucose levels in your blood rise which is how you develop prediabetes. If that process is not stopped and is allowed to progress, you will develop type 2 diabetes. Being overweight and eating an unhealthy diet increases your risk of becoming resistant to insulin.
Not everyone with prediabetes has symptoms. Early signs of prediabetes can include:
- increased thirst
- increased hunger
- needing to urinate (pee/mimi) often
- feeling very tired.
If you have noticed some or all of these symptoms, or have any of the risk factors for diabetes, visit your healthcare provider for a blood glucose check.
There are a few blood tests that can diagnose prediabetes. The most common test is called HbA1c, which measure the amount of glucose that has built up in your blood over a 3-month period. Other tests include a fasting blood glucose and a glucose tolerance test. Read more about how diabetes and prediabetes are diagnosed.
The age at which you should be tested for prediabetes depends on your ethnicity, family history and other medical history. This is because diabetes is more common in Māori, Pasifika and South Asian (eg, Indian, Pakistani, Sri Lankan) ethnicities, people who are overweight and people who have whānau members with diabetes. Read more about who should be screened for diabetes.
People with prediabetes are also at increased risk of developing diabetes complications, so it needs to be treated. Read more about complications of diabetes.
Prediabetes is treated mainly by changing your lifestyle where needed. This could delay you developing diabetes by 3–4 years or even prevent you developing it at all. Healthy lifestyles are made up of healthy eating, active living, having a healthy body weight and being smoke free.
Other treatments for prediabetes can include:
- Diabetes medicine – if lifestyle changes don’t lead to your blood glucose levels reducing enough, your healthcare provider may consider prescribing metformin.
- Treating other cardiovascular risk factors such as high blood pressure and high blood fats (eg, cholesterol).
If you have prediabetes, it's important to have an HbA1c test every year to check whether you have progressed to type 2 diabetes.
Lifestyle management
Healthy eating
- There is no special prediabetes diet. Like everyone, you can follow Michael Pollan's advice to “Eat food. Not too much. Mostly plants”.
- Healthy eating is not about sticking to strict diets or depriving yourself of the foods you love.
- Instead, eat a wide range of different foods, mostly plant-based and less processed, that help you feel great, have more energy, improve your outlook and achieve or maintain a healthy weight.
- Find out more healthy eating basics and advice from the New Zealand Society for the Study of Diabetes on healthy eating.(external link)(external link)
Active living
- Regular physical activity, sitting less and moving more can help you have a healthy body weight, feel more positive and lower your risk of diabetes, heart disease and some cancers.
- Physical activity also really helps your body to use insulin properly.
- Try not to sit down for longer than 30 minutes at a time.
- Aim to be active for at least 30 minutes every day, increasing to 60 minutes daily if you want to reduce your body weight.
- A good intensity level is to feel your heart rate go up and experience heavier breathing, but still be able to speak a sentence.
- Include some resistance exercise at least twice a week.
- Doing some physical activity is still better than doing none.
- Make sure you wear comfortable, supportive and well-fitting shoes as you are at greater risk of foot problems if you have prediabetes or diabetes.
- If you find it hard to start or maintain an exercise routine, talk to your healthcare provider as you may be able to get a green prescription to access support.
- Find out more about physical activity.
A healthy body weight
- If you are overweight or obese, losing 5–10% of your initial body weight can significantly improve your blood glucose, reduce your risk of developing diabetes, and reduce your blood pressure and cholesterol.
- Making good choices about what you eat and drink, and being physically active will help you achieve and keep a healthy body weight.
Be smoke free
If you are a smoker, quitting smoking is also important.
Alcohol
If you drink alcohol, try to reduce your intake as it contains a lot of calories and can make weight management more difficult. Regular heavy drinking can also make your body resist insulin which can trigger type 2 diabetes.
The best things you can do to prevent prediabetes are:
- maintaining a healthy body weight
- making healthy food and drink choices
- doing regular physical activity.
Diabetes support groups Diabetes self-management support groups or programmes are available in some areas. Ask your healthcare provider about what’s available in your area.
The following links provide further information about prediabetes. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Prediabetes(external link) Diabetes NZ Auckland Branch
Prediabetes(external link) HealthInfo Canterbury, NZ
JumpStart(external link) Exercise, nutrition and support programme for people with diabetes and prediabetes
Diabetes NZ(external link)
Resources
80% of type 2 diabetes is preventable [PDF, 1.2 MB] Healthify He Puna Waiora, 2019
Pre-diabetes(external link) Diabetes NZ, 2014
Diabetes prevention [PDF, 422 KB] Auckland DHB and Diabetes Projects Trust, NZ, 2011 Amharic [PDF, 1.4 MB], Arabic [PDF, 1.1 MB], Chinese [PDF, 1.2 MB], Dari [PDF, 793 KB], English [PDF, 422 KB], Hindi [PDF, 1.1 MB], Korean [PDF, 1.2 MB], te reo Māori [PDF, 3.2 MB], Samoan [PDF, 1.2 MB], Tongan [PDF, 1.2 MB], Vietnamese [PDF, 1.2 MB]
Diabetes & healthy food choices(external link) Diabetes NZ, 2019 English(external link), Chinese(external link)
Here’s healthy food(external link) Diabetes NZ, 2014
Love don't judge(external link) Diabetes New Zealand
References
- Prediabetes(external link) Ministry of Health, NZ & NZ Society for the Study of Diabetes, 2020
- Prediabetes – risk factor management(external link) Ministry of Health, NZ, 2016
- HbA1c testing Healthify He Puna Waiora, NZ
- Endoscopic weight loss program(external link) John Hopkins Medicine, US
Clinical guidelines and resources
Best Practice diabetes toolbox(external link) BPAC, NZ, 2021
Type 2 diabetes management guidance(external link) NZ Society for the Study of Diabetes and Ministry of Health, NZ, 2021
Prediabetes – risk factor management(external link) Ministry of Health, NZ, 2016
Initiating interventions in people with intermediate hyperglycaemia ("pre-diabetes")(external link) BPAC, NZ, 2012
General practice toolkit for more heart and diabetes checks and better help for smokers to quit(external link) Ministry of Health, NZ, 2014
NZ diabetes and obesity(external link) Research Review, NZ
NZ Primary Care Handbook 2012(external link) Ministry of Health, NZ, 2012
Hemmingsen B, Gimenez-Perez G, Mauricio D, Roqué i Figuls M, Metzendorf MI, Richter B. Diet, physical activity or both for prevention or delay of type 2 diabetes mellitus and its associated complications in people at increased risk of developing type 2 diabetes mellitus(external link) Cochrane Database of Systematic Reviews. 2017;12:CD003054.
See our page Diabetes for healthcare providers
Continuing professional development
Podcast
Prediabetes(external link) Goodfellow Podcast, 2019
Professor Bruce Arroll discusses prediabetes and preventing progression to type 2 diabetes. Bruce is a GP in South Auckland, Director of the Goodfellow Unit and a Professor in General Practice at the University of Auckland.
Brochures

Healthify He Puna Waiora, NZ and Mediboard, 2023
Diabetes NZ, 2014
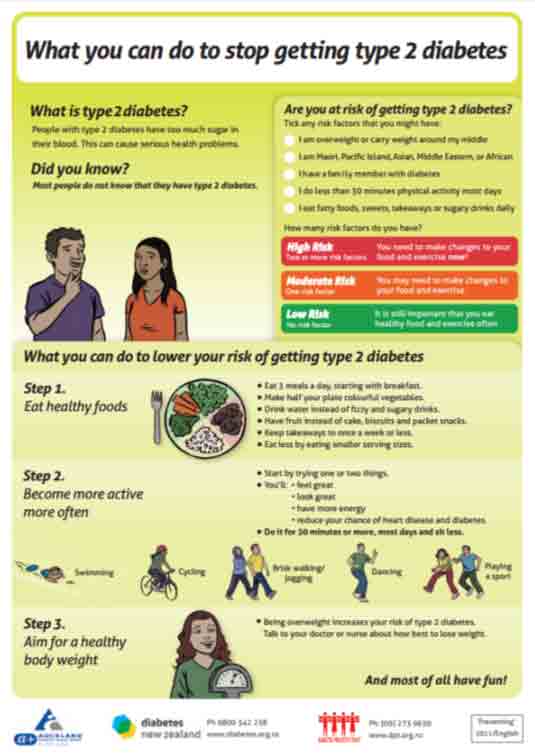
Auckland DHB and Diabetes Projects Trust, NZ, 2011
Amharic, Arabic, Chinese, Dari, English, Hindi, Korean, te reo Māori, Samoan, Tongan, Vietnamese.Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Associate Professor Sue Wells, Public Health Physician, University of Auckland
Last reviewed:
Page last updated:





