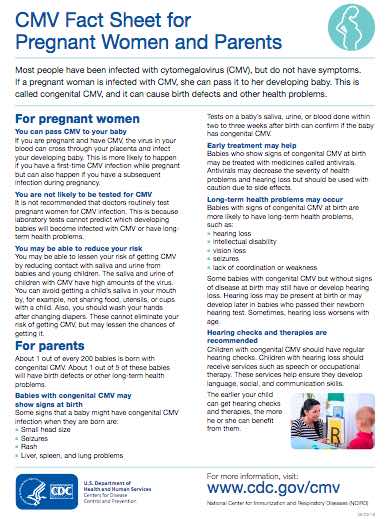
CMV is a virus. It is mainly spread through being in close contact with someone who already has it. It can be passed on through body fluids including saliva, blood and urine.
CMV can only be passed on when it is ‘active’. This is when:
- you catch the virus for the first time – young children often get CMV for the first time when they start early childhood education
- the virus has been re-activated because you have a weakened immune system
- you’ve been re-infected with a different strain (type) of CMV.
Once you have it, it stays in your body for the rest of your life.