|
See your doctor or go to the nearest emergency department immediately if you, or someone you care for, experience the following: |
|
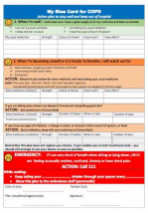
- Signs of a flare-up include coughing or wheezing more, producing more phlegm or mucus than usual, a change in the colour and consistency of your phlegm, experiencing more shortness of breath (trouble breathing) than usual and feeling more tired.
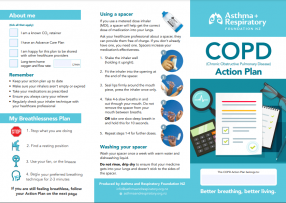
- The best way to manage a COPD flare-up is to have a COPD action plan and use your medicines as described in the plan.
- A COPD action plan is a written document that provides you with instructions and information on how to manage your COPD on a daily basis. It also tells you how to recognise and cope with worsening symptoms (exacerbations).
- You can develop your COPD action plan with your healthcare provider and set it up to suit the severity of your COPD and your preferences.