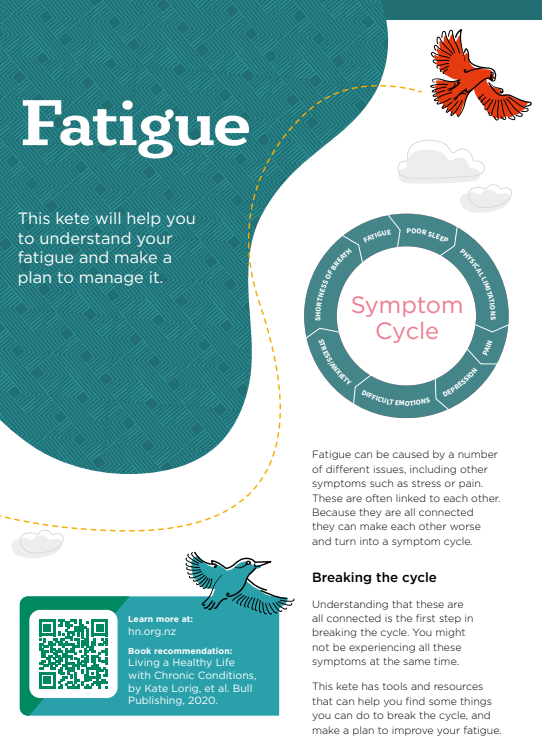
- ME/CFS is a complex illness that affects many systems of your body, particularly the nervous and immune systems.
- People with ME/CFS experience extreme tiredness that doesn't go away with rest and can’t be explained by other causes.
- Other symptoms may include muscle pain, sleep problems, poor concentration, headaches and a drop in blood pressure when standing.
- Diagnosis can be difficult as the symptoms are similar to many other conditions and there are no specific tests for it.
- There's no specific treatment for ME/CFS, but there are things that can be done to help manage your symptoms.
- ME/CFS is not well understood and health professionals are still learning about the best ways to manage the symptoms.
- There's a lot of disagreement, and people often have very strong feelings about how to manage ME/CFS..
- This page provides a basic introduction to this topic, in-depth discussion is beyond its scope.
Low or no data? Visit zero.govt.nz, scroll down the page then click on our logo to return to our site and browse for free.
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)
Also known as Tapanui flu, post-viral syndrome
Key points about myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)
- ME/CFS is a complex illness that affects many systems of your body, particularly the nervous and immune systems.
- People with ME/CFS experience extreme tiredness that doesn't go away with rest and other symptoms relating to pain, sleep, concentration and blood pressure.
- ME/CFS isn't well understood. Diagnosis can be difficult and there's no specific treatment.
- Experts disagree on how to manage the condition, but there are things you can do to manage your symptoms.
- This page provides a basic introduction to this controversial topic.

The cause of ME/CFS is not yet fully understood, but it's likely that several factors contribute to its development. It's associated with changes in the immune system and body chemistry.
ME/CFS is usually triggered by a viral infection, eg, glandular fever or influenza, but any infection may be the trigger. The ongoing effects of COVID-19 infection, known as long COVID, are very similar to the symptoms of ME/CFS.
It's possible that the potential for getting ME/CFS is genetic and runs in families.
Other factors that may contribute include:
- emotional or physical distress
- not enough sleep
- hormonal imbalance
- over-exercising.
People with ME/CFS experience overwhelming physical and mental fatigue (tiredness). This is different to the tiredness that people who are well experience after strenuous exercise or a day's work. ME/CFS-associated fatigue can be debilitating and doesn't readily get better with rest.
Other common symptoms include:
- poor memory or concentration
- sore throat
- tender lymph nodes
- muscle pain
- multiple joint pain without joint swelling or redness
- headaches of a new type, pattern or severity
- unrefreshing sleep
- tiredness that can last for more than 24 hours after physical or mental effort.
Some people also report a range of other symptoms including:
- sensitivities to food, medicine or alcohol
- trouble regulating temperature (feeling cold, hot having night sweats)
- gastrointestinal problems – nausea (feeling sick), loss of appetite, irritable bowel syndrome (IBS), bloating, diarrhoea (runny poo)
- sensitivity to light or noise
- feeling breathless during physical activity
- difficulty with being upright (eg, blood pressure changes, dizziness).
The severity of symptoms can vary from day to day, or even within a day.
The following video is one person's story of his ME/CFS journey. There has loud music at the start, if this is a problem you could turn down the volume for a few seconds.
Note that people experience ME/CFS differently and some may have much more severe symptoms than described in the video.
Video: Living with CFS/ME – Alun's story
Experts and organisations sometimes differ in their definition of ME/CFS.
Diagnosis can be difficult because the symptoms of ME/CFS are similar to those of a number of other medical conditions, which need to be ruled out first. There are no specific tests available to make the diagnosis which depends on the kinds of symptoms someone has, how severe they are and how long they've been present.
Most ME/CFS organisations, researchers and doctors have agreed that for a diagnosis of ME/CFS to be made:
- Symptoms should be present for at least 6 months in adults and more than 3 months in children (although symptoms for shorter periods can still be ME/CFS) and include:
- severe fatigue that's new, significantly limits your ability to function, and can't be explained by another medical condition
- significant fatigue or malaise after physical or mental exertion
- unrefreshing sleep, and
- problems with cognition (eg, confusion, difficulty concentrating, memory loss) or
- difficulty standing up because of signs or symptoms that get better when you're lying down.
If you're experiencing these symptoms, your healthcare provider may use more detailed and accurate criteria based on an ME/CFS diagnostic questionnaire to confirm the diagnosis.
The severity of symptoms can vary widely so the diagnosis may range from mild ME/CFS to severe ME/CFS as follows:
- Mild – you can move about, can care for yourself and do light housework with difficulty. You may be well enough to work, attend school or study, if you have learnt to pace yourself carefully.
- Moderate – you have reduced ability and are restricted in most activities of daily living. You are likely to have stopped work or education and have poor sleep.
- Severe – you are unlikely to be able to do very much for yourself, spend much of your time in bed and may depend on a wheelchair. You are also likely to have severe problems thinking, remembering or concentrating, and be sensitive to light and noise.
As there is no treatment that can cure ME/CFS the condition is 'treated' by treating or managing the symptoms experienced.
Management plan
A management plan for ME/CFS aims to relieve your symptoms to improve your quality of life. The plan could include:
- how to manage stress
- a very gentle exercise plan personally designed to help you maintain muscle strength but not bring on a worsening of symptoms (known as post-exertional malaise or PEM)
- a nutritious diet, with regular meals/snacks to keep up your energy
- supplements, if your diet lacks a good balance or if your blood tests indicate deficiencies
- a sleep management plan, which may include medicine
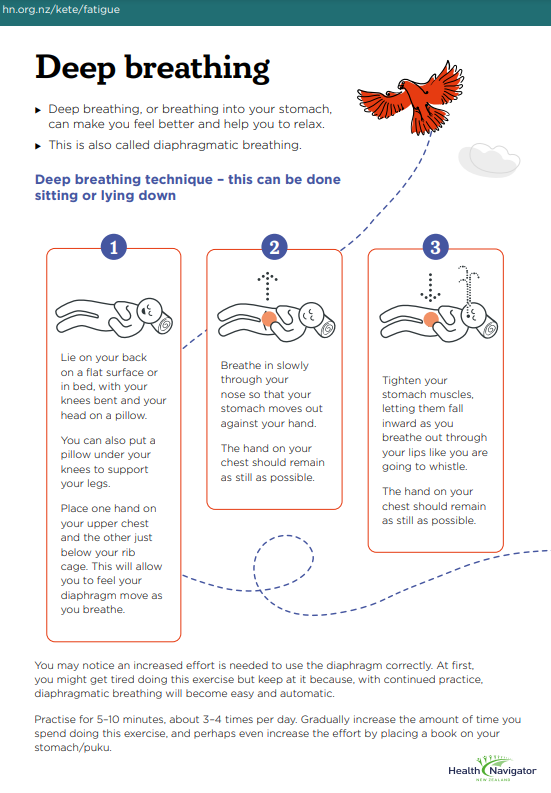
- physiotherapy to help with pain and good breathing techniques
- medicine for pain
- psychological input if you are particularly stressed or depressed. Counselling, psychotherapy, cognitive behavioural therapy and group therapy can all be helpful.
Note: the use of some treatment approaches is controversial, and experts differ in their opinions about what works and doesn’t.
Complementary and alternative medicines and therapies are often tried for ME/CFS. It’s a good idea to talk through your plans with your healthcare provider.
The important thing is that you build a good relationship with a healthcare provider you trust, and work out a plan together that suits you and your circumstances.
Medicines
There are medicines that may be used to relieve some of the symptoms.
Over-the-counter painkillers occasionally can help ease headaches as well as muscle and joint pain. Your healthcare provider may prescribe stronger painkillers, although they should only be used on a short-term basis. You may be referred to a pain management clinic if you have long-term pain or fibromyalgia, which can look a lot like ME/CFS.
People with ME/CFS usually have poor sleep, and medicine may improve your sleep quality and give you a better chance of recovery.
Antidepressants can be important for people with ME/CFS who are experiencing depression or anxiety as a result of living with the condition. Talk to your healthcare provider about whether these might be useful for you.
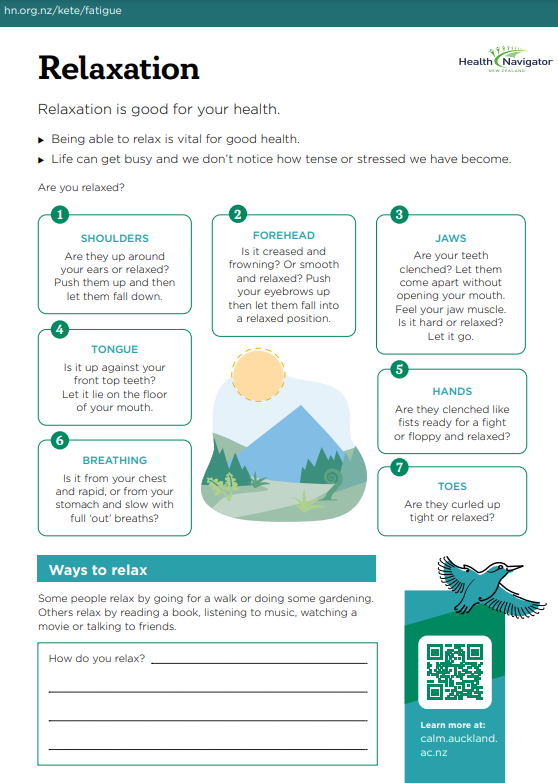
Things you can do to help manage this condition include:.
- learning about ME/CFS(external link)
- reducing your stress
- getting plenty of rest
- making sleep a priority – if you're having trouble sleeping, here are some tips to improve your sleeping habits
- eating a healthy diet to make sure your body is getting the nutrients it needs
- having plenty of salt if you have low blood pressure and a tendency to feel dizzy or even faint on standing (common in people with ME/CFS)
- learning to prioritise the things you need to get done, and then pacing yourself by dividing them into short times of activity with rest breaks in between
- learning mindfulness, meditation or creative visualisation
- getting out into nature regularly, listening to music and enjoying your pets
- developing a support network of understanding friends and whānau for when you need help
- joining a support group(external link) if there is one in your area or an online group if not (see the support section below)
- talking to your healthcare provider about whether there are any medicines or supplements that may help you.
- Take along a list of all the symptoms you're experiencing in case you forget some of them during your talk with the doctor or nurse.
- Talk about how much you can do at work or school and around the house.
- Ask if there are any financial supports or services (eg, home help or personal care support) you could apply for.
- Ask for help with pain, sleep and staying active if these are problems for you.
- Ask about what you should be eating.
The long-term outlook varies quite a bit. There may be times when your symptoms are not too bad and other times when they flare up and become worse. However, many people improve over time (over months and years rather than weeks) and some recover well. Children and younger people have a better rate of full recovery.
Early diagnosis and treatment may lessen the impact of the illness. The important thing to remember is that this is not a progressive or life-threatening disease and that for many people full recovery is possible.
There are many myths out there about ME/CFS that can be harmful to patients with this condition. Some of these include:
People with ME/CFS are just tired
The facts: People with ME/CFS experience overwhelming physical and mental exhaustion. This is different to how you feel after you've had a few nights of poor sleep or the feeling you get after strenuous exercise. Just getting a good night’s sleep is not going to make them feel better.
ME/CFS is not a real disease
The facts: ME/CFS is recognized as a unique disease by all major medical groups worldwide. Research is showing that patients with ME/CFS may have changes to their immune, endocrine (gland) and metabolic function, among others, compared with people who don't have it. There may also be a genetic component to the disease.
Not many people are affected by ME/CFS
The facts: In Aotearoa New Zealand, it's estimated that at least 25,000 people experience ME/CFS, which means more people are affected by ME/CFS than by multiple sclerosis.
ME/CFS only causes tiredness
The facts: ME/CFS can cause other symptoms including a sore throat, muscle pain, tender lymph nodes and impaired memory or concentration.
Only women get ME/CFS
The facts: Men get ME/CFS too, and children are also affected. The female to male ratio is 70:30 and the most common age of onset is 33–55 years.
- The Associated NZ ME Society (ANZMES) has support groups(external link) around the country.
- M.E. Awareness NZ(external link) provides information about available support.
- ME Support(external link) is a charity helping New Zealanders with ME/CFS and their whānau or carers.
- Complex Chronic Illness Support(external link) Phone 07 281 1481. Information, support and practical advice for people, families and carers affected by ME/CFS.
What is ME (CFS)?(external link) The Associated NZ ME Society (ANZMES)
Management of CFS(external link) Dr Rosamund Vallings, NZ
The art and science of pacing for ME(external link) M.E. Awareness NZ
ME/CFS(external link) Centers for Disease Control and Prevention, US
Brochures
Preparing to discuss ME/CFS with a healthcare provider(external link) Centers for Disease Control and Prevention, US
On the day of your office visit for ME/CFS(external link) Centers for Disease Control and Prevention, US
After a healthcare provider visit for ME/CFS(external link) Centers for Disease Control and Prevention, US
References
- What is ME?(external link) The Associated NZ ME Society
- Long COVID(external link) Ministry of Health, NZ, 2023
- Myalgic encephalomyelitis/chronic fatigue syndrome(external link) Patient Info, UK, 2021
- Chronic fatigue syndrome(external link) Auckland Regional HealthPathways, NZ, 2018
- Myalgic encephalomyelitis/Chronic fatigue syndrome(external link) 3D HealthPathways, NZ, 2021
- Friedberg F et al. Chronic fatigue syndrome/myalgic encephalyitis – a primer for clinical practitioners(external link)(external link) International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (IACFS/ME), 2014
- What is ME/CFS?(external link) Emerge, Australia
- Management of CFS(external link) Dr Rosamund Vallings, NZ
- ME/CFS(external link) Centers for Disease Control and Prevention, US, 2023
Brochures
Healthify He Puna Waiora, NZ, 2022
Healthify He Puna Waiora, NZ, 2022
Healthify He Puna Waiora, NZ, 2022
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Healthify Clinical Advisors
Last reviewed:





