The nervous system in your body consists of the central nervous system (CNS) and the peripheral nervous system (PNS). The central nervous system is made up of your brain and spinal cord. The peripheral nervous system is made up of nerves that carry messages from your brain and spinal cord to other parts of your body.
The peripheral nerves have motor and sensory nerves. Motor nerves carry messages from your brain and spinal cord to your muscles, telling them to contract. Sensory nerves carry stimuli such as touch and pain in the form of signals to your brain and spinal cord.
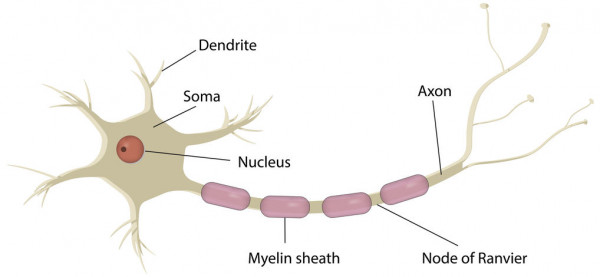
Image credit: 123rf
A peripheral nerve's structure can be seen in the image above. The axon is similar to the wiring of an electric cable that transmits messages between our brain and spinal cord and the rest of your body. The myelin sheath wraps around the axon and acts as a protection layer, similar to the insulation of a cable, to make sure electrical messages are not broken while they are being sent.
In CMT, the myelin sheath and axon of peripheral nerves are damaged. This is due to faulty genes. There are many different types of CMT that are caused by different faulty changes in your genes. The main types of CMT include:
- CMT 1
- CMT 2
- CMT 3
- CMT 4
- CMT X.
Read more about the types and classification of CMT(external link)(external link).
If you have CMT, you may have inherited faulty genes from one or both of your parents.






