- Bulimia can affect people of any gender and at any age. It is most likely to develop during your late teens or early twenties, and it is more common among women.
- Binge eating involves eating a large amount of food in a short space of time, often feeling as though you are out of control, and also feeling shame and guilt.
- Behaviours to make up for the effects of binge eating can include vomiting, fasting, excessive exercise, misusing laxatives, diuretics and prescription medication, or illegal drug use.
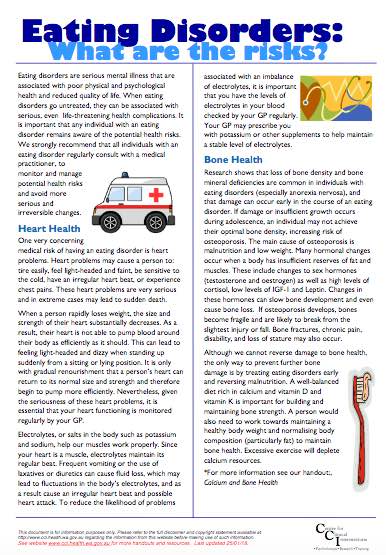
- Bulimia can affect the long-term health of your teeth, digestive system, hormones, fertility, heart and kidney function.
- People with bulimia over-value the importance of their body weight or shape in determining their self-worth.
- If you get treatment from an eating disorder specialist, you have a very good chance of getting better, even if you have had this condition for a long time.
(NHS, UK, 2020)