You can't catch Bx or give Bx to anyone. Bx is different from asthma but some children with Bx have asthma as well.
Bronchiectasis (Bx) is a chest disease – the airways in the lungs have become damaged and scarred.
The airways (or breathing tubes) become widened and mucus can be trapped in pockets within the airway. Having extra mucus in the airways means bacteria and viruses can grow quickly and cause infections.
These infections cause damage and more scarring to the airways and lungs. Once this has happened, the scarring is usually lifelong. But, with good treatment, there can be some improvement and further damage prevented. Good treatment is especially important in young children because their lungs are still growing.
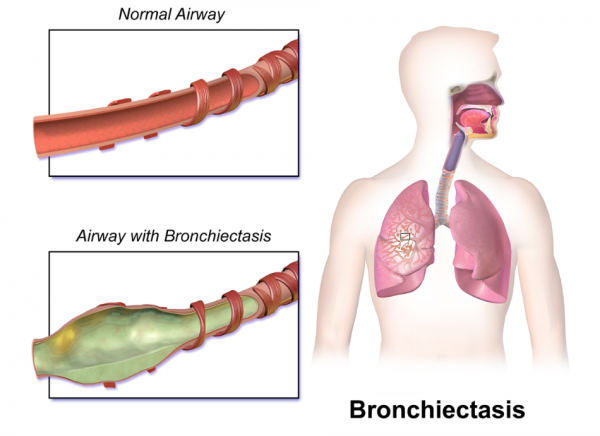
Image credit: BruceBlaus, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons
Video: Cough-free – the way to be
The following video features former Warriors rugby league player Wairangi Koopu. It focuses on recognising the signs of infection that can lead to bronchiectasis, and acting on them. This video may take a few moments to load.