We don’t know exactly what causes bowel polyps. They grow in the lower part of your bowel – the large intestine (colon) and the rectum (the lower part before your bottom.) The lining of your bowel is always renewing itself. Polyps happen when one area grows more than it should. This is sometimes because of a problem with the genes (inherited from your family) which control growth of the cells lining your bowel.
Below is a picture of your gastrointestinal system with the colon shown as the darker pink part at the left and top of the small intestine. The inserted image at the top shows a bowel polyp.
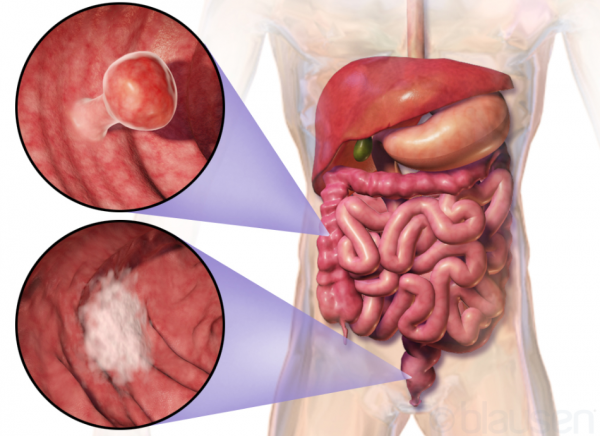
Image credit: Blausen.com Wikimedia Commons






