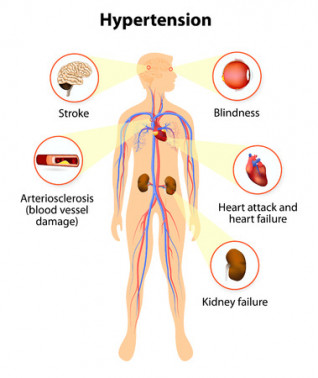
High blood pressure is one of the most common health problems as people get older. With a little effort, there is much you can do to reduce your risk of getting high blood pressure and the increased risk of stroke and heart disease that goes with that.
Keep to a healthy body weight
One of the key risk factors for high blood pressure is being overweight. Being overweight(external link) can make you 2 to 6 times more likely to develop high blood pressure than being in the normal weight range. Even small amounts of weight loss(external link) can make a big difference in helping to prevent and treat high blood pressure.
Be active regularly
People who are physically active have a lower risk of getting high blood pressure (20–50% lower) than people who are not active. Even light activities, if done daily, can help lower your risk. Add more activity to your day. Aim to get 30 to 60 minutes of physical activity most days of the week. Walking, cycling and swimming are ideal. Find an activity you enjoy so you can keep it up.
Look for opportunities to add a few minutes here and there – it all helps. Take the stairs whenever you can, park 5 minutes further from work, go for a walk at lunchtime or when you get home. Read more about getting active.
Eat a balanced diet
Your diet – what you eat and drink – has a real effect on your heart and blood pressure. The more healthy your eating habits are, the lower your blood pressure will be. A heart healthy diet is low in saturated fat, whole grains, 8 servings of coloured vegetables and fruit, and 2 to 3 servings of low-fat milk or milk products a day. Read more about healthy eating.
Eat less salt
Cutting back on salt also helps prevent your blood pressure from rising. Reduce your sodium intake to 2300mg of sodium a day (about 6g salt) or less. This includes sodium from processed food. Use herbs, spices, fruit and vinegar for flavouring and dressings. If you have pre-prepared foods, avoid pickled food and avoid salty or fatty takeaway foods. Read more about reducing your salt intake [PDF, 255 KB].
Limit how much alcohol you drink
Drinking too much alcohol can raise your blood pressure. Limit how much alcohol you drink and follow recommended guidelines for low-risk drinking.
Quit smoking
Being smokefree is one of the best things you can do to lower your risk of heart attack and stroke. While smoking does not directly affect your blood pressure, it will cause your arteries to narrow just as high blood pressure does. This puts you at much higher risk of heart disease and stroke.
So, if you smoke and have high blood pressure, your arteries will narrow much more quickly and your risk of a heart attack or stroke in the future is dramatically increased. Because of this, as well as for all the other effects it has on your health, it well worth giving up smoking. Read more about quitting smoking.
Reduce stress
Stress can make blood pressure go up, and over time may contribute to the cause of high blood pressure. There are many steps you can take to reduce your stress. Read more about managing stress.
Avoid eating large quantities of liquorice
Liquorice contains a chemical that can raise blood pressure. Eating more than 57g of black liquorice a day for at least 2 weeks could lead to potentially serious health problems, such as an increase in blood pressure and an irregular heart rhythm (arrhythmia).
For most people, liquorice found in foods is safe to eat and safe when consumed in small amounts for short periods of time.